


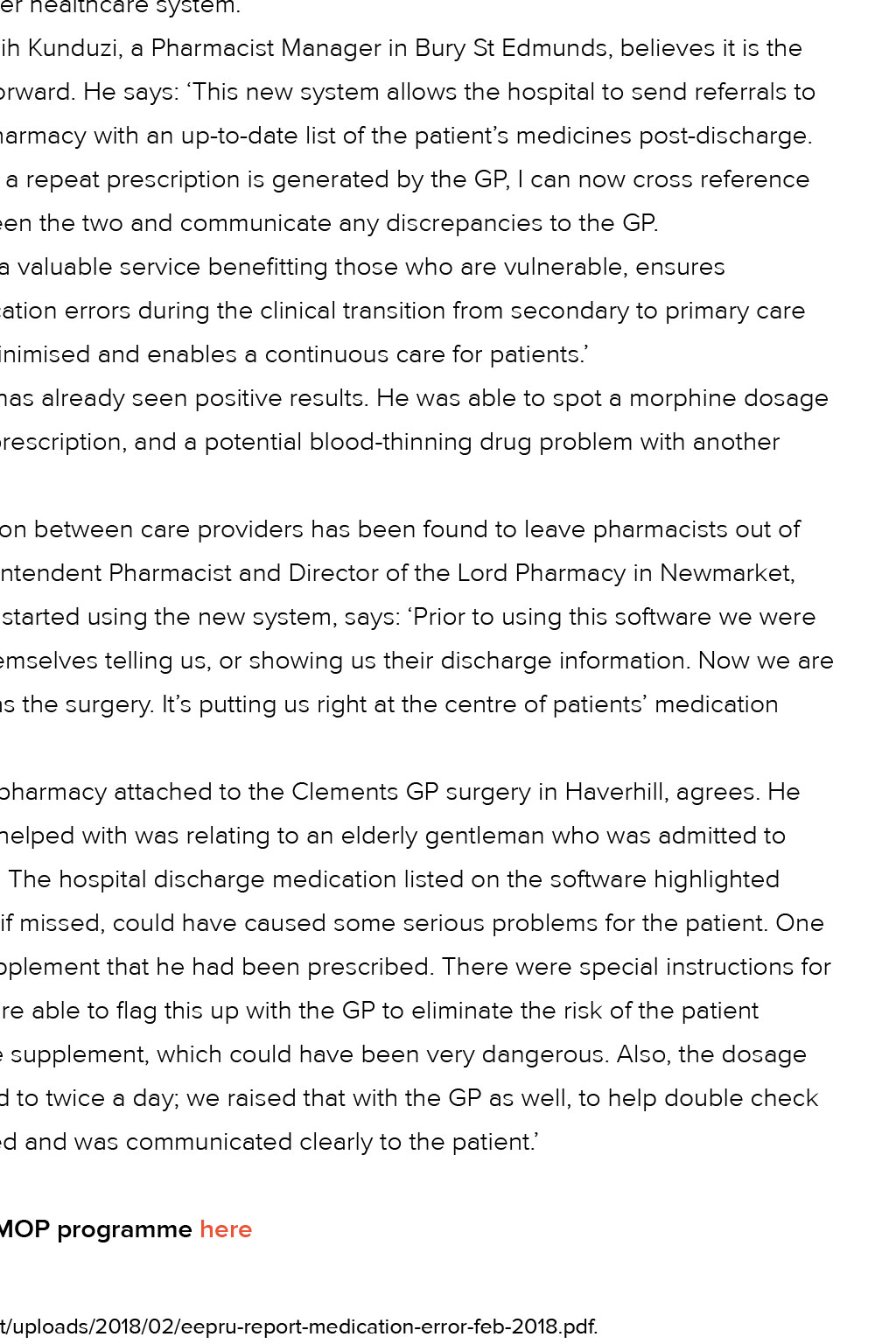





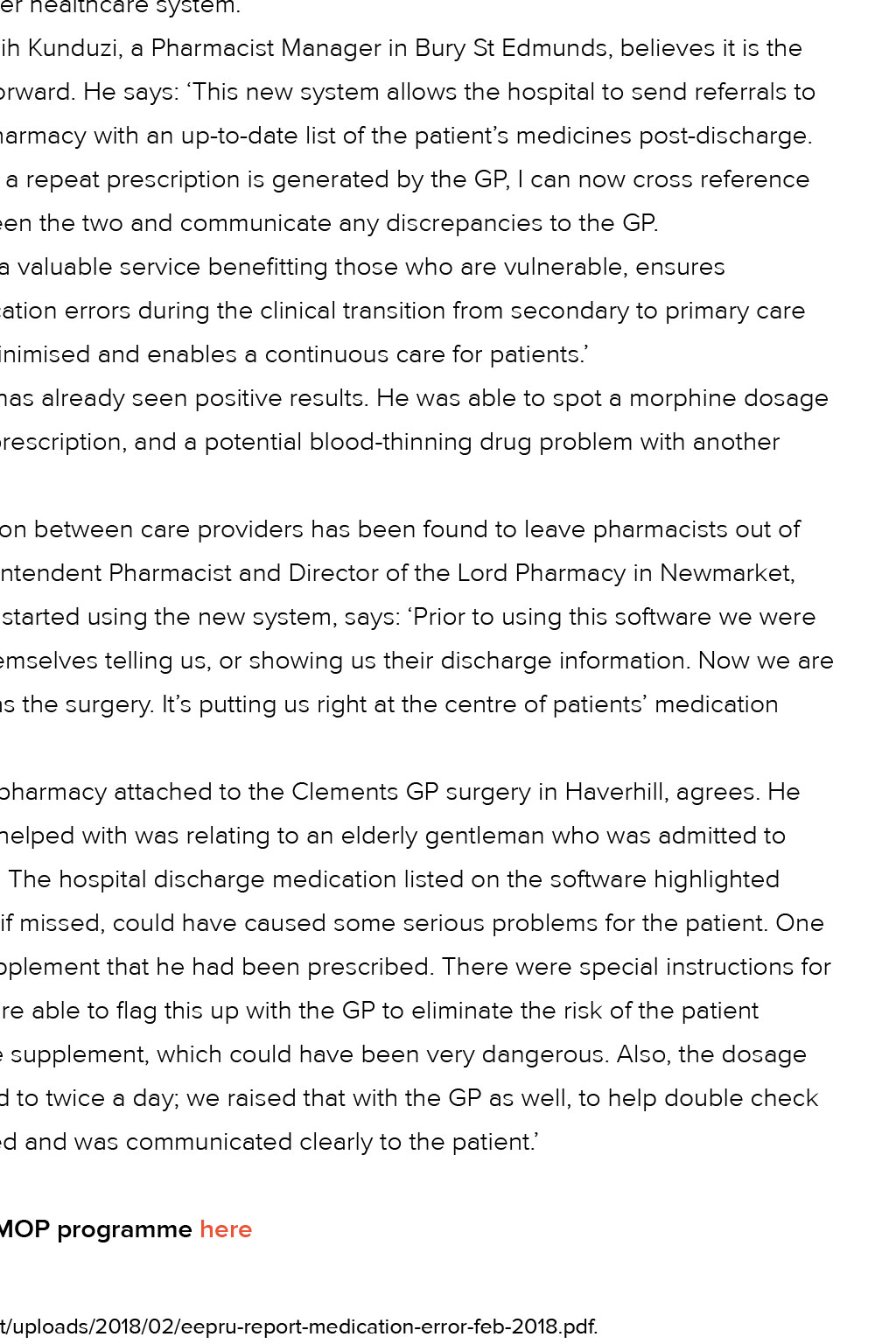


Patient safety: Electronic Medicines Optimisation Pathway On the right (Rx) course More than 1,800 people have benefited from a new initiative to help pharmacists spot mistakes and make a real difference to patient safety Research estimates that 237 million medication errors occur annually at any point at which a patient comes into contact with a drug – including prescribing, dispensing, administering and monitoring – while almost 75 per cent are unlikely to result in harm to patients. Those errors that are clinically significant, with potential to cause moderate or Seven trusts are benefifiting pharmacist faster, more accurately and is a more efficient process for health professionals and patients. The programme is making a real difference for patients and it offers community pharmacists a chance to use their clinical skills and to be an integral part of the patient pathway. It enables them to have a closer professional relationship with their patients and to plan their workload better when hospital patients are discharged. It also delivers savings for the healthcare system by reducing the number of hospital admissions and freeing up beds. With support from NHS trusts, Local Pharmaceutical Committees (LPCs), and Sustainability and Transformation Partnerships (STPs), Eastern AHSN has facilitated implementation of technology and supported pathway change in trusts and community pharmacies, funding licence costs, helping to engage and train community pharmacists, as well as supporting programme management and communications. Community pharmacists actioned 1,824 referrals sent by hospital pharmacies during the year, extending the benefits for patients and the broader healthcare system. Masih Kunduzi, a Pharmacist Manager in Bury St Edmunds, believes it is the way forward. He says: ‘This new system allows the hospital to send referrals to the pharmacy with an up-to-date list of the patient’s medicines post-discharge. When a repeat prescription is generated by the GP, I can now cross reference between the two and communicate any discrepancies to the GP. ‘It’s a valuable service benefiting those who are vulnerable, ensures medication errors during the clinical transition from secondary to primary care are minimised and enables a continuous care for patients.’ severe harm, constitute 25.8 per cent and 2.0 per cent of overall errors, respectively. For patients being discharged from hospital, it can mean the difference between them experiencing a smooth transition to home or having to face an emergency re-admission. To help improve this, Eastern AHSN has been implementing the national Electronic Medicines Optimisation Pathway (EMOP) programme in the East of England. The programme aims to reduce the risk of unintentional changes to patient treatment on discharge from an acute trust to primary care. EMOP is providing a more efficient way for hospital pharmacy teams to send updated medication discharge information details electronically to a patient’s community pharmacist, so they can get prompt advice about any prescription changes. The programme ensures that information reaches the community 1 He has already seen positive results. He was able to spot a morphine dosage error on one woman’s repeat prescription, and a potential blood-thinning drug problem with another patient. Inefficiencies in communication between care providers has been found to leave pharmacists out of the loop in some cases. Superintendent Pharmacist and Director of the Lord Pharmacy in Newmarket, Zuzer Musaji who has recently started using the new system, says: ‘Prior to using this software we were often reliant on the patients themselves telling us, or showing us their discharge information. Now we are getting information as quickly as the surgery. It’s putting us right at the centre of patients’ medication management.’ David Holland, owner of the pharmacy attached to the Clements GP surgery in Haverhill, agrees. He explains: ‘One case that it has helped with was relating to an elderly gentleman who was admitted to hospital with cardiac problems. The hospital discharge medication listed on the software highlighted some significant changes that, if missed, could have caused some serious problems for the patient. One was relating to a potassium supplement that he had been prescribed. There were special instructions for the next three days and we were able to flag this up with the GP to eliminate the risk of the patient accidentally carry on taking the supplement, which could have been very dangerous. Also, the dosage of his diuretic pill had increased to twice a day; we raised that with the GP as well, to help double check that the change had been noted and was communicated clearly to the patient.’ ● Find out more about our EMOP programme here Footnotes 1 http://www.eepru.org.uk/wp-content/uploads/2018/02/eepru-report-medication-error-feb-2018.pdf. Patient safety: Electronic Medicines Optimisation Pathway More than 1,800 people have benefited from a new initiative to help pharmacists spot mistakes and make a real difference to patient safety Research estimates that 237 million medication errors occur annually at any point at which a patient comes into contact with a drug – including prescribing, dispensing, administering and monitoring – while almost 75 per cent are unlikely to result in harm to patients. Those errors that are clinically significant, with potential to cause moderate or Seven trusts are benefifiting pharmacist faster, more accurately and is a more efficient process for health professionals and patients. The programme is making a real difference for patients and it offers community pharmacists a chance to use their clinical skills and to be an integral part of the patient pathway. It enables them to have a closer professional relationship with their patients and to plan their workload better when hospital patients are discharged. It also delivers savings for the healthcare system by reducing the number of hospital admissions and freeing up beds. With support from NHS trusts, Local Pharmaceutical Committees (LPCs), and Sustainability and Transformation Partnerships (STPs), Eastern AHSN has facilitated implementation of technology and supported pathway change in trusts and community pharmacies, funding licence costs, helping to engage and train community pharmacists, as well as supporting programme management and communications. Community pharmacists actioned 1,824 referrals sent by hospital pharmacies during the year, extending the benefits for patients and the broader healthcare system. Masih Kunduzi, a Pharmacist Manager in Bury St Edmunds, believes it is the way forward. He says: ‘This new system allows the hospital to send referrals to the pharmacy with an up-to-date list of the patient’s medicines post-discharge. When a repeat prescription is generated by the GP, I can now cross reference between the two and communicate any discrepancies to the GP. ‘It’s a valuable service benefiting those who are vulnerable, ensures medication errors during the clinical transition from secondary to primary care are minimised and enables a continuous care for patients.’ severe harm, constitute 25.8 per cent and 2.0 per cent of overall errors, respectively. For patients being discharged from hospital, it can mean the difference between them experiencing a smooth transition to home or having to face an emergency re-admission. To help improve this, Eastern AHSN has been implementing the national Electronic Medicines Optimisation Pathway (EMOP) programme in the East of England. The programme aims to reduce the risk of unintentional changes to patient treatment on discharge from an acute trust to primary care. EMOP is providing a more efficient way for hospital pharmacy teams to send updated medication discharge information details electronically to a patient’s community pharmacist, so they can get prompt advice about any prescription changes. The programme ensures that information reaches the community 1 He has already seen positive results. He was able to spot a morphine dosage error on one woman’s repeat prescription, and a potential blood-thinning drug problem with another patient. Inefficiencies in communication between care providers has been found to leave pharmacists out of the loop in some cases. Superintendent Pharmacist and Director of the Lord Pharmacy in Newmarket, Zuzer Musaji who has recently started using the new system, says: ‘Prior to using this software we were often reliant on the patients themselves telling us, or showing us their discharge information. Now we are getting information as quickly as the surgery. It’s putting us right at the centre of patients’ medication management.’ David Holland, owner of the pharmacy attached to the Clements GP surgery in Haverhill, agrees. He explains: ‘One case that it has helped with was relating to an elderly gentleman who was admitted to hospital with cardiac problems. The hospital discharge medication listed on the software highlighted some significant changes that, if missed, could have caused some serious problems for the patient. One was relating to a potassium supplement that he had been prescribed. There were special instructions for the next three days and we were able to flag this up with the GP to eliminate the risk of the patient accidentally carry on taking the supplement, which could have been very dangerous. Also, the dosage of his diuretic pill had increased to twice a day; we raised that with the GP as well, to help double check that the change had been noted and was communicated clearly to the patient.’ ● Find out more about our EMOP programme here Footnotes 1 http://www.eepru.org.uk/wp-content/uploads/2018/02/eepru-report-medication-error-feb-2018.pdf. On the right (Rx) course Seven trusts are benefifiting Eastern AHSN has supported seven trusts across Essex, Hertfordshire and Suffolk to go live with EMOP: ● Basildon and Thurrock University Hospitals NHS Foundation Trust ● East and North Hertfordshire NHS Trust ● West Suffolk NHS Foundation Trust ● Mid Essex Hospital Services NHS Trust ● East Suffolk and North Essex NHS Foundation Trust ● Southend University Hospital NHS Foundation Trust ● The Princess Alexandra Hospital NHS Trust