

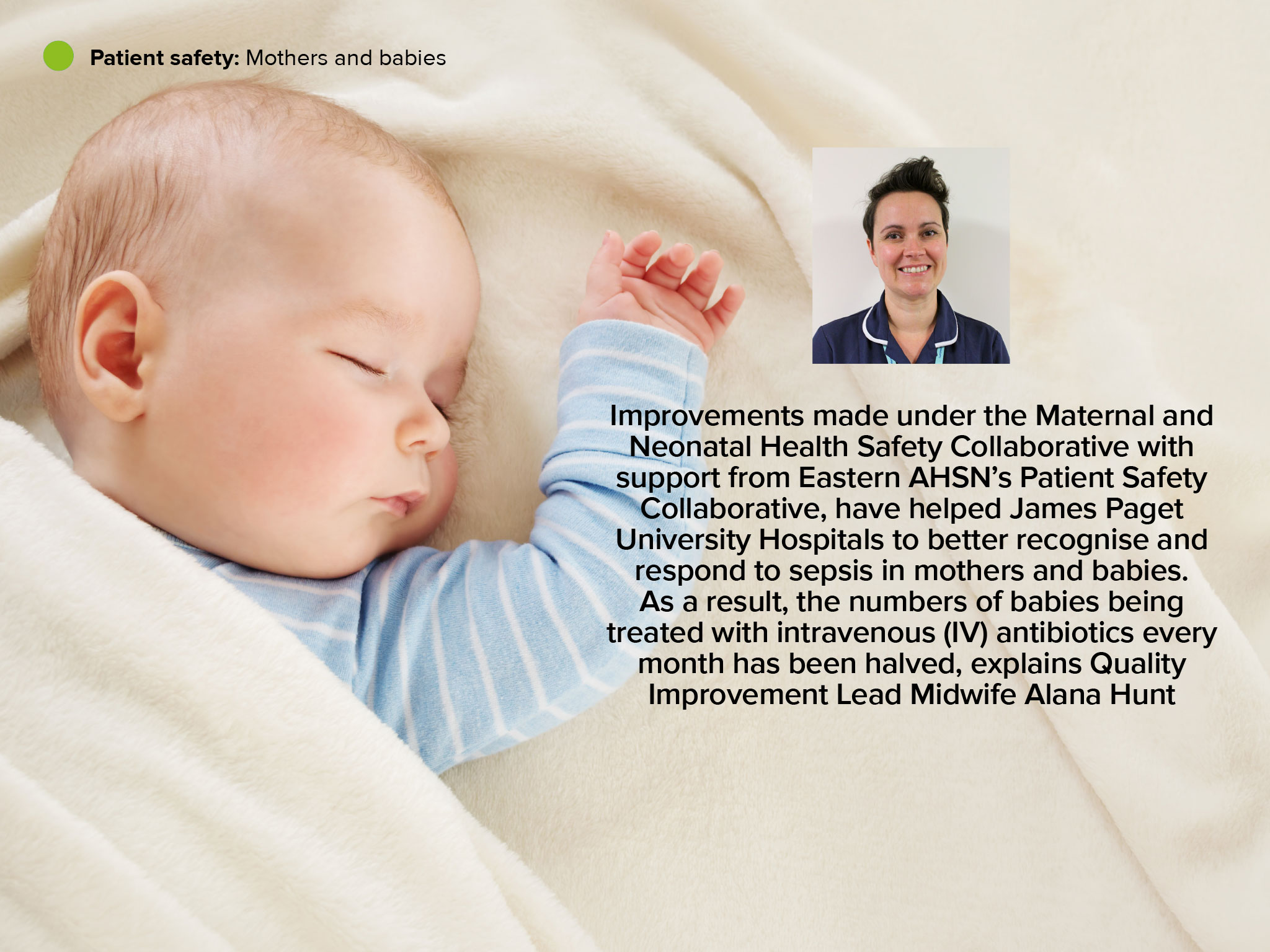
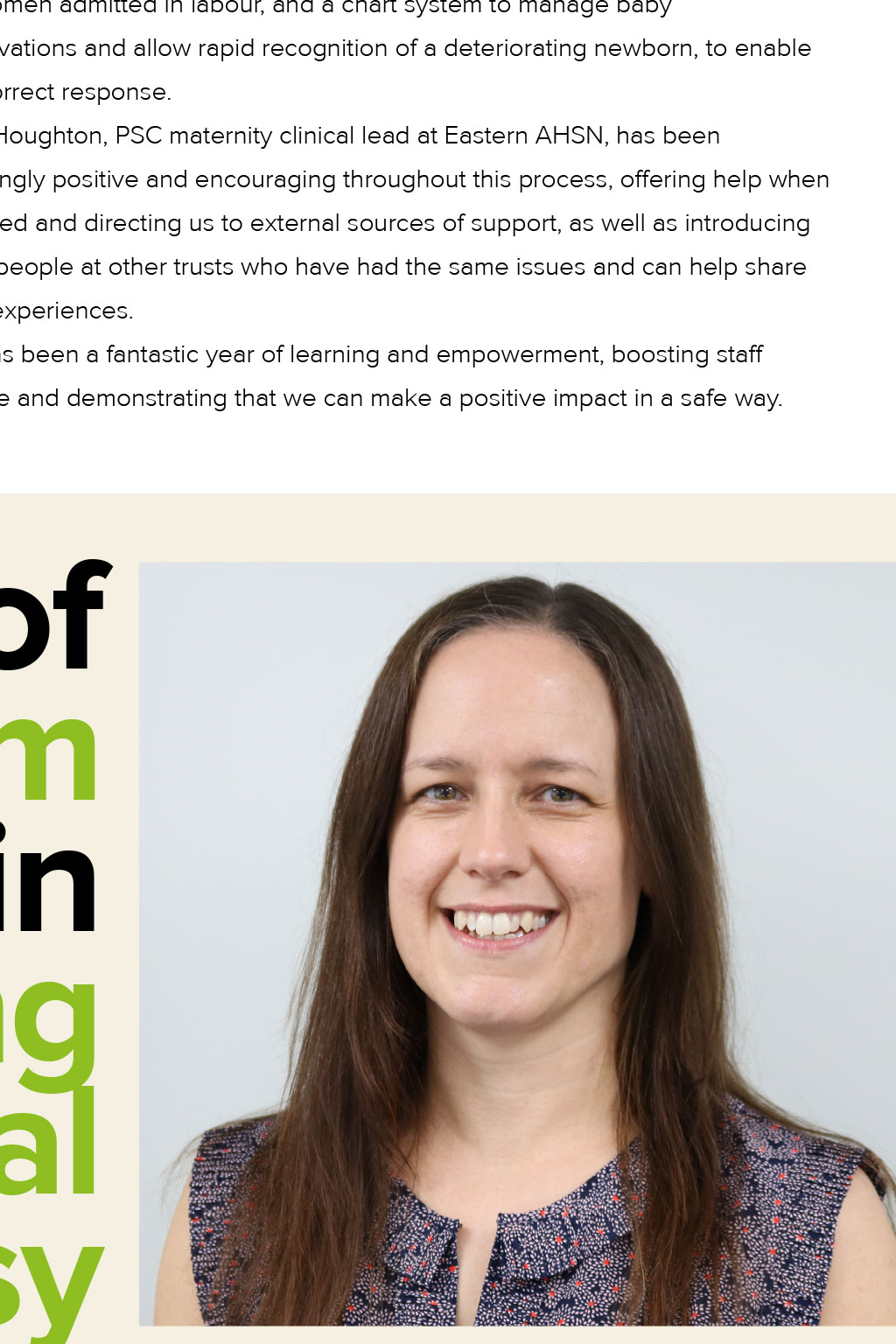
Patient safety: Mothers and babies Improvements made under the Maternal and Neonatal Health Safety Collaborative with support from Eastern AHSN’s Patient Safety Collaborative, have helped James Paget University Hospitals to better recognise and respond to sepsis in mothers and babies. As a result, the numbers of babies being treated with intravenous (IV) antibiotics every month has been halved, explains Quality Improvement Lead Midwife Alana Hunt Reducing sepsis in maternity units Keeping mums and babies together We have just completed one year of the maternity and neonatal programme which aims to help NHS maternity units embed quality improvement methods to reduce the number of maternity and neonatal deaths, stillbirths and brain injuries that occur during or shortly after birth by 20 per cent by 2020. We decided to focus on reducing the number of babies being admitted to the neonatal unit with suspected sepsis and cases of babies being treated with IV antibiotics. The trust’s baseline data showed that we could make significant improvements in the prevention, recognition and treatment of sepsis for both newborns babies and labouring mothers. One of the many challenges was helping our teams to adjust to a change of culture in the way they managed sepsis for women in labour and their babies that would enable wherever possible mothers and babies to be kept together in a safe way. Consistent communication with our staff was key, with information shared at meetings, in face-to-face discussions and on posters. We also held a sepsis awareness day and a QI training session at our monthly midwifery days. As a result of our staff’s commitment, we have: ● Reduced the number of women requiring antibiotic treatment in labour, by focusing on prevention ● Improved our recognition of sepsis and how we treat it ● Halved the number of babies with risk factors for sepsis receiving IV antibiotics. Before the collaboration with Eastern AHSN, we were treating about 20 babies per month with IV antibiotics, which we’ve halved to 10 and maintained at that level over the last few months One of the ways we focused on prevention was by testing pyrexia prevention stickers. Pyrexia, a raised body temperature of more than 37.5°C, in labour is the biggest trigger factor for antibiotic treatment for mothers, which can lead to their babies receiving the same medication. Recognising that a woman’s temperature can naturally rise during childbirth without any sepsis or infection present, our aim was to avoid unnecessary treatment. We also introduced a guideline to separate treatment of infection from sepsis in labour, meaning many babies avoided unnecessary antibiotics. As well as reviewing our processes, we have tested a risk-assessment tool for women admitted in labour, and a chart system to manage baby observations and allow rapid recognition of a deteriorating newborn, to enable the correct response. Jill Houghton, PSC maternity clinical lead at Eastern AHSN, has been amazingly positive and encouraging throughout this process, offering help when required and directing us to external sources of support, as well as introducing us to people at other trusts who have had the same issues and can help share their experiences. It has been a fantastic year of learning and empowerment, boosting staff morale and demonstrating that we can make a positive impact in a safe way. The role of magnesium sulphate in preventing cerebral palsy Women at risk of pre-term labour are the target audience for NHS programme, says Dr Sam O’Hare, Consultant Neonatologist at Cambridge University Hospitals NHS Foundation Trust and Regional Neonatal Lead for PReCePT As a neonatal consultant, I look after newborn babies, many of whom are born prematurely. The earlier a baby is born, the higher their risk of developing cerebral palsy. The condition is typically caused by damage to the brain that occurs before, during or soon after birth, and it can lead to lifelong challenges. Some children are mildly affected, while others have severe movement problems and learning difficulties that have a huge impact on their life and that of their family. Studies have shown that giving magnesium sulphate (MgSO4) to women at risk of pre-term birth can help reduce the chance of their child developing cerebral palsy by around 30 per cent. Dr Sam O’Hare talks about the programe NHS England’s PReCePT programme – Prevention of Cerebral Palsy in Pre-term Labour – aims to increase the number of eligible women who are given magnesium sulphate before they give birth. At Eastern AHSN, we are working closely with maternity units across our region to raise awareness of this national initiative and to encourage mums and their babies to benefit. Across the region, approximately 20 women a month are eligible to receive antenatal MgSO4. For every 37 mothers who receive treatment, one case of cerebral palsy is prevented. All 11 maternity units in the Eastern region now have a PReCePT lead midwife to raise awareness and train staff so that these women can be identified early and given magnesium sulphate before they give birth. It is a very cost-effective intervention, with an ampoule of the drug costing only £1. A bolus dose is given by intravenous injection, followed by an IV infusion, which is run continuously for up to 24 hours until the baby is born. Midwives have been working hard to adopt the programme in this region, and Anneka Burch, PReCePT Lead Midwife at Ipswich Hospital, said: “I am proud to be leading the project within my hospital, sharing the knowledge I have gained with my colleagues, with the aim of making a difference to premature babies and their families.” Patient safety: Mothers and babies Improvements made under the Maternal and Neonatal Health Safety Collaborative with support from Eastern AHSN’s Patient Safety Collaborative, have helped James Paget University Hospitals to better recognise and respond to sepsis in mothers and babies. As a result, the numbers of babies being treated with intravenous (IV) antibiotics every month has been halved, explains Quality Improvement Lead Midwife Alana Hunt Keeping mums and babies together We have just completed one year of the maternity and neonatal programme which aims to help NHS maternity units embed quality improvement methods to reduce the number of maternity and neonatal deaths, stillbirths and brain injuries that occur during or shortly after birth by 20 per cent by 2020. We decided to focus on reducing the number of babies being admitted to the neonatal unit with suspected sepsis and cases of babies being treated with IV antibiotics. The trust’s baseline data showed that we could make significant improvements in the prevention, recognition and treatment of sepsis for both newborns babies and labouring mothers. One of the many challenges was helping our teams to adjust to a change of culture in the way they managed sepsis for women in labour and their babies that would enable wherever possible mothers and babies to be kept together in a safe way. Consistent communication with our staff was key, with information shared at meetings, in face-to-face discussions and on posters. We also held a sepsis awareness day and a QI training session at our monthly midwifery days. As a result of our staff’s commitment, we have: ● Reduced the number of women requiring antibiotic treatment in labour, by focusing on prevention ● Improved our recognition of sepsis and how we treat it ● Halved the number of babies with risk factors for sepsis receiving IV antibiotics. Before the collaboration with Eastern AHSN, we were treating about 20 babies per month with IV antibiotics, which we’ve halved to 10 and maintained at that level over the last few months One of the ways we focused on prevention was by testing pyrexia prevention stickers. Pyrexia, a raised body temperature of more than 37.5°C, in labour is the biggest trigger factor for antibiotic treatment for mothers, which can lead to their babies receiving the same medication. Recognising that a woman’s temperature can naturally rise during childbirth without any sepsis or infection present, our aim was to avoid unnecessary treatment. We also introduced a guideline to separate treatment of infection from sepsis in labour, meaning many babies avoided unnecessary antibiotics. As well as reviewing our processes, we have tested a risk-assessment tool for women admitted in labour, and a chart system to manage baby observations and allow rapid recognition of a deteriorating newborn, to enable the correct response. Jill Houghton, PSC maternity clinical lead at Eastern AHSN, has been amazingly positive and encouraging throughout this process, offering help when required and directing us to external sources of support, as well as introducing us to people at other trusts who have had the same issues and can help share their experiences. It has been a fantastic year of learning and empowerment, boosting staff morale and demonstrating that we can make a positive impact in a safe way. The role of magnesium sulphate in preventing cerebral palsy Women at risk of pre-term labour are the target audience for NHS programme, says Dr Sam O’Hare, Consultant Neonatologist at Cambridge University Hospitals NHS Foundation Trust and Regional Neonatal Lead for PReCePT As a neonatal consultant, I look after newborn babies, many of whom are born prematurely. The earlier a baby is born, the higher their risk of developing cerebral palsy. The condition is typically caused by damage to the brain that occurs before, during or soon after birth, and it can lead to lifelong challenges. Some children are mildly affected, while others have severe movement problems and learning difficulties that have a huge impact on their life and that of their family. Studies have shown that giving magnesium sulphate (MgSO4) to women at risk of pre-term birth can help reduce the chance of their child developing cerebral palsy by around 30 per cent. Dr Sam O’Hare talks about the programe NHS England’s PReCePT programme – Prevention of Cerebral Palsy in Pre-term Labour – aims to increase the number of eligible women who are given magnesium sulphate before they give birth. At Eastern AHSN, we are working closely with maternity units across our region to raise awareness of this national initiative and to encourage mums and their babies to benefit. Across the region, approximately 20 women a month are eligible to receive antenatal MgSO4. For every 37 mothers who receive treatment, one case of cerebral palsy is prevented. All 11 maternity units in the Eastern region now have a PReCePT lead midwife to raise awareness and train staff so that these women can be identified early and given magnesium sulphate before they give birth. It is a very cost-effective intervention, with an ampoule of the drug costing only £1. A bolus dose is given by intravenous injection, followed by an IV infusion, which is run continuously for up to 24 hours until the baby is born. Midwives have been working hard to adopt the programme in this region, and Anneka Burch, PReCePT Lead Midwife at Ipswich Hospital, said: “I am proud to be leading the project within my hospital, sharing the knowledge I have gained with my colleagues, with the aim of making a difference to premature babies and their families.” Reducing sepsis in maternity units Keeping mums and babies together Mothers and babies have a psychological and physiological need to be kept together at the moment of birth and during the hours and days that follow. Keeping mothers and babies together is a safe and healthy birth practice1 and there is increasing evidence that early emotional interactions between a baby and their parents, particularly the mother, are fundamental to brain development, subsequent success, life chances and the ability to form strong loving relationships2 Footnotes 1 Crenshaw, 2007. 2 Gerhardt 2004; Bystrova et al 2009; Howard et al 2011. Patient safety: Mothers and babies Improvements made under the Maternal and Neonatal Health Safety Collaborative with support from Eastern AHSN’s Patient Safety Collaborative, have helped James Paget University Hospitals to better recognise and respond to sepsis in mothers and babies. As a result, the numbers of babies being treated with intravenous (IV) antibiotics every month has been halved, explains Quality Improvement Lead Midwife Alana Hunt Reducing sepsis in maternity units Keeping mums and babies together We have just completed one year of the maternity and neonatal programme which aims to help NHS maternity units embed quality improvement methods to reduce the number of maternity and neonatal deaths, stillbirths and brain injuries that occur during or shortly after birth by 20 per cent by 2020. We decided to focus on reducing the number of babies being admitted to the neonatal unit with suspected sepsis and cases of babies being treated with IV antibiotics. The trust’s baseline data showed that we could make significant improvements in the prevention, recognition and treatment of sepsis for both newborns babies and labouring mothers. One of the many challenges was helping our teams to adjust to a change of culture in the way they managed sepsis for women in labour and their babies that would enable wherever possible mothers and babies to be kept together in a safe way. Consistent communication with our staff was key, with information shared at meetings, in face-to-face discussions and on posters. We also held a sepsis awareness day and a QI training session at our monthly midwifery days. As a result of our staff’s commitment, we have: ● Reduced the number of women requiring antibiotic treatment in labour, by focusing on prevention ● Improved our recognition of sepsis and how we treat it ● Halved the number of babies with risk factors for sepsis receiving IV antibiotics. Before the collaboration with Eastern AHSN, we were treating about 20 babies per month with IV antibiotics, which we’ve halved to 10 and maintained at that level over the last few months One of the ways we focused on prevention was by testing pyrexia prevention stickers. Pyrexia, a raised body temperature of more than 37.5°C, in labour is the biggest trigger factor for antibiotic treatment for mothers, which can lead to their babies receiving the same medication. Recognising that a woman’s temperature can naturally rise during childbirth without any sepsis or infection present, our aim was to avoid unnecessary treatment. We also introduced a guideline to separate treatment of infection from sepsis in labour, meaning many babies avoided unnecessary antibiotics. As well as reviewing our processes, we have tested a risk-assessment tool for women admitted in labour, and a chart system to manage baby observations and allow rapid recognition of a deteriorating newborn, to enable the correct response. Jill Houghton, PSC maternity clinical lead at Eastern AHSN, has been amazingly positive and encouraging throughout this process, offering help when required and directing us to external sources of support, as well as introducing us to people at other trusts who have had the same issues and can help share their experiences. It has been a fantastic year of learning and empowerment, boosting staff morale and demonstrating that we can make a positive impact in a safe way. The role of magnesium sulphate in preventing cerebral palsy Women at risk of pre-term labour are the target audience for NHS programme, says Dr Sam O’Hare, Consultant Neonatologist at Cambridge University Hospitals NHS Foundation Trust and Regional Neonatal Lead for PReCePT As a neonatal consultant, I look after newborn babies, many of whom are born prematurely. The earlier a baby is born, the higher their risk of developing cerebral palsy. The condition is typically caused by damage to the brain that occurs before, during or soon after birth, and it can lead to lifelong challenges. Some children are mildly affected, while others have severe movement video box developing cerebral palsy by around 30 per cent. NHS England’s PReCePT programme – Prevention of Cerebral problems and learning difficulties that have a huge impact on their life and that of their family. Studies have shown that giving magnesium sulphate (MgSO4) to women at risk of pre-term birth can help reduce the chance of their child Dr Sam O’Hare talks about the programe Palsy in Pre-term Labour – aims to increase the number of eligible women who are given magnesium sulphate before they give birth. At Eastern AHSN, we are working closely with maternity units across our region to raise awareness of this national initiative and to encourage mums and their babies to benefit. Across the region, approximately 20 women a month are eligible to receive antenatal MgSO4. For every 37 mothers who receive treatment, one case of cerebral palsy is prevented. All 11 maternity units in the Eastern region now have a PReCePT lead midwife to raise awareness and train staff so that these women can be identified early and given magnesium sulphate before they give birth. It is a very cost-effective intervention, with an ampoule of the drug costing only £1. A bolus dose is given by intravenous injection, followed by an IV infusion, which is run continuously for up to 24 hours until the baby is born. Midwives have been working hard to adopt the programme in this region, and Anneka Burch, PReCePT Lead Midwife at Ipswich Hospital, said: “I am proud to be leading the project within my hospital, sharing the knowledge I have gained with my colleagues, with the aim of making a difference to premature babies and their families.”