


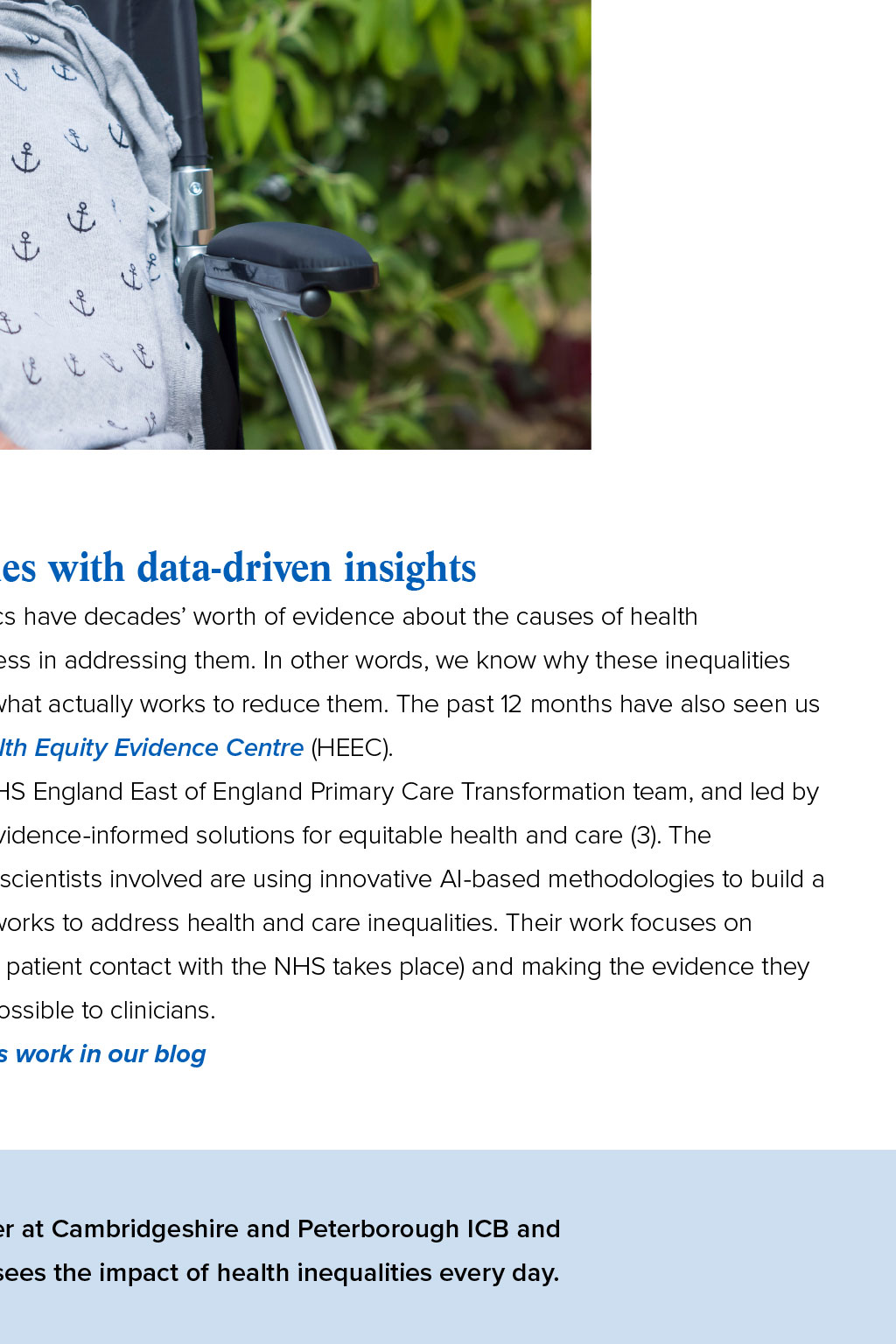
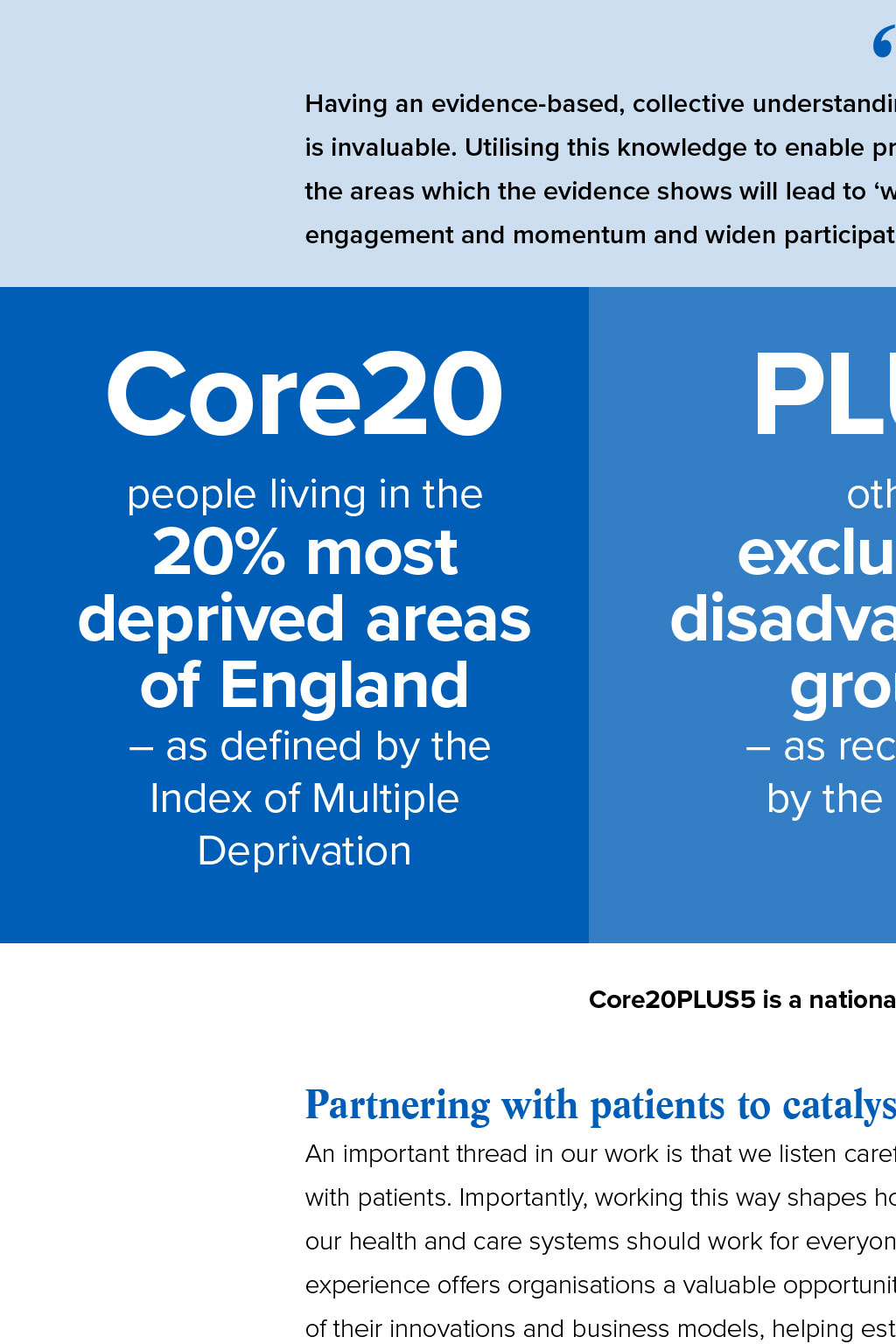
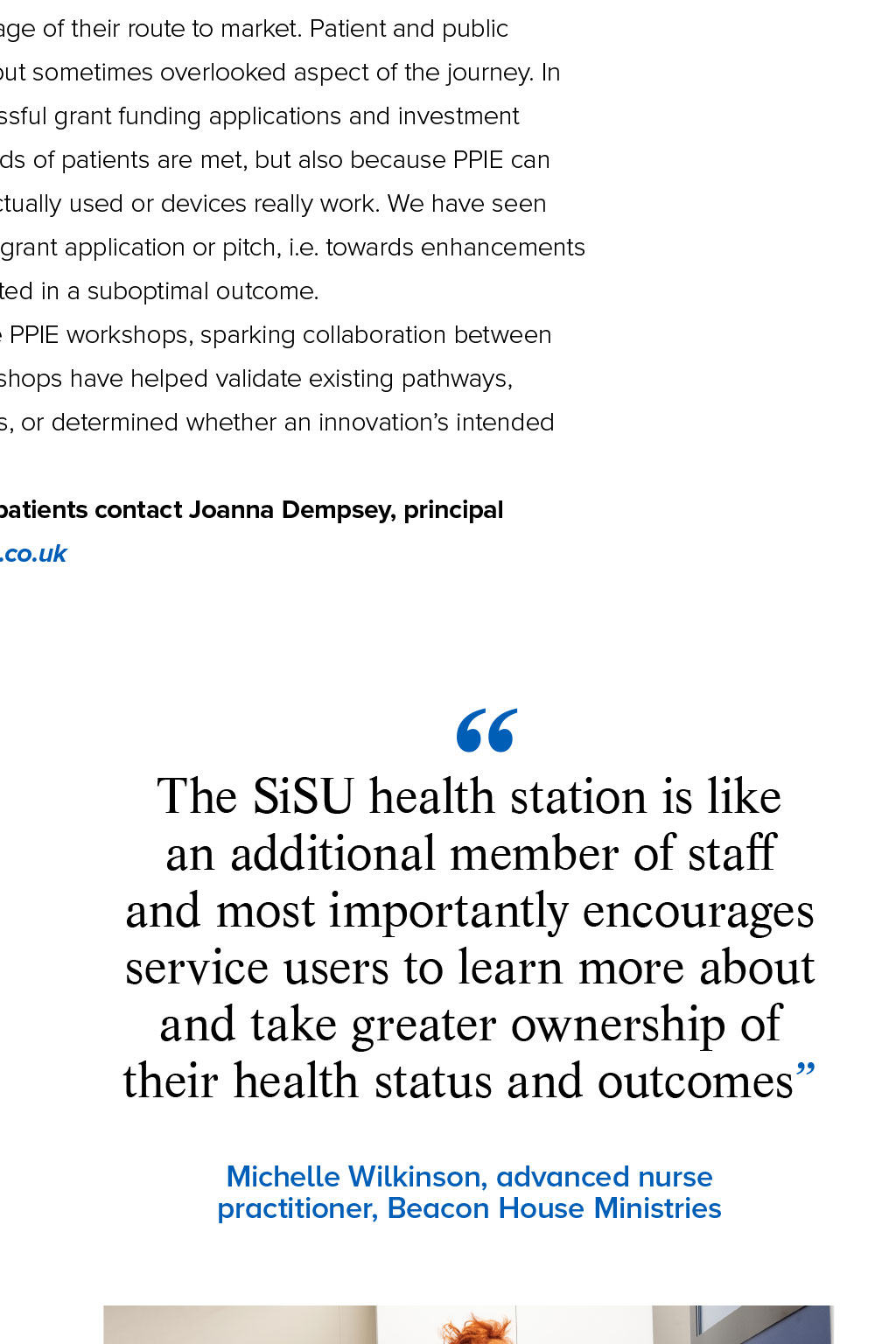




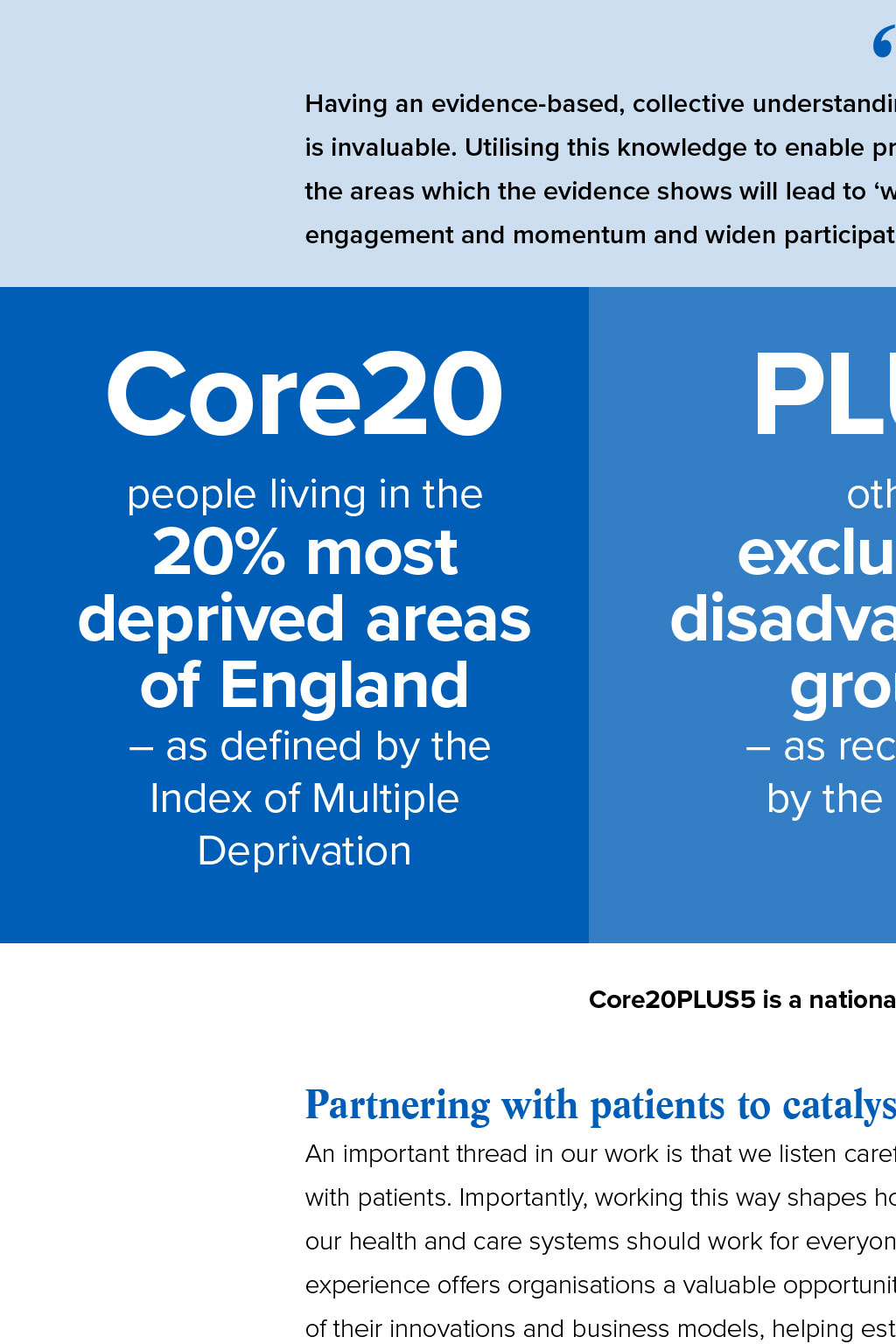
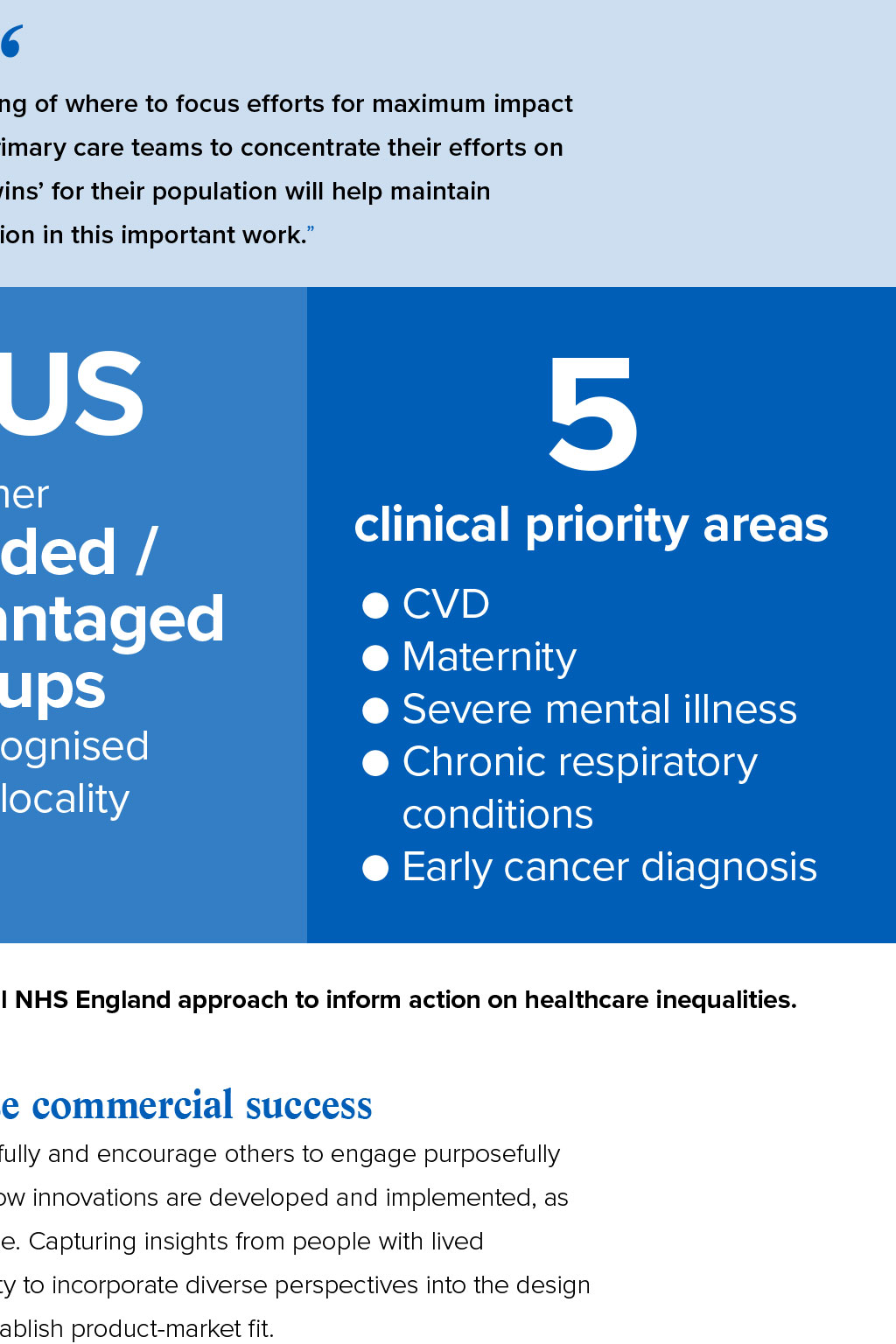
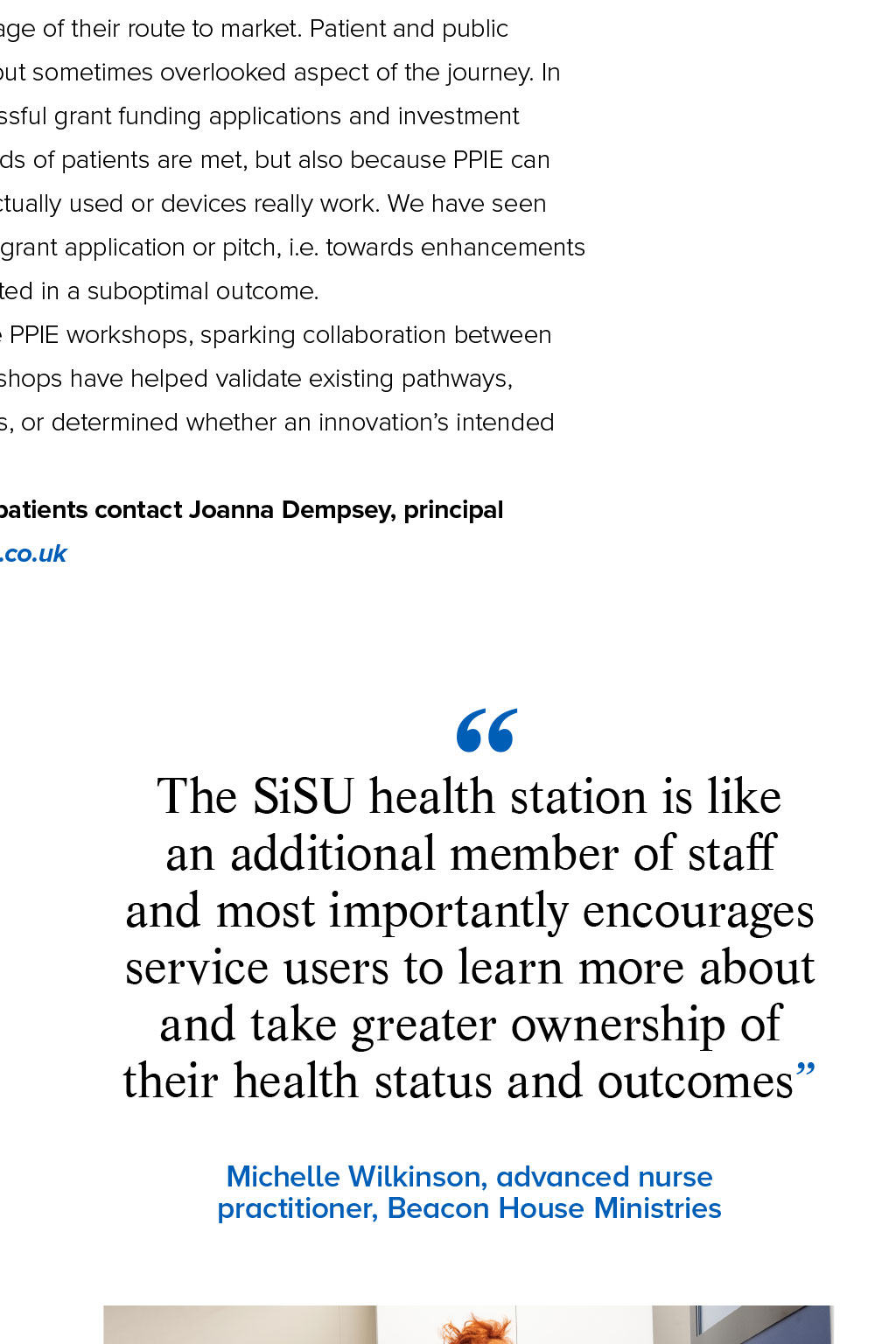
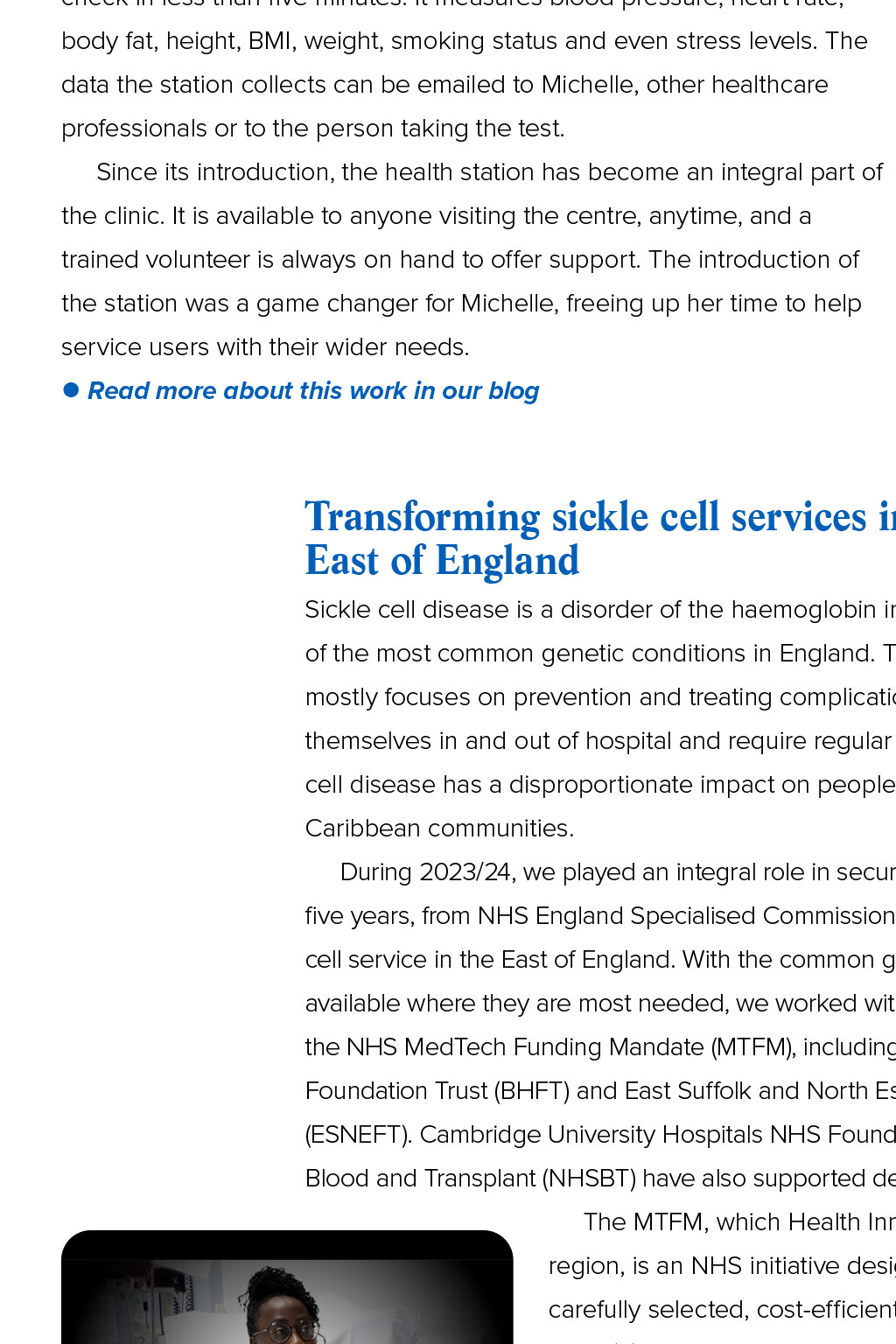
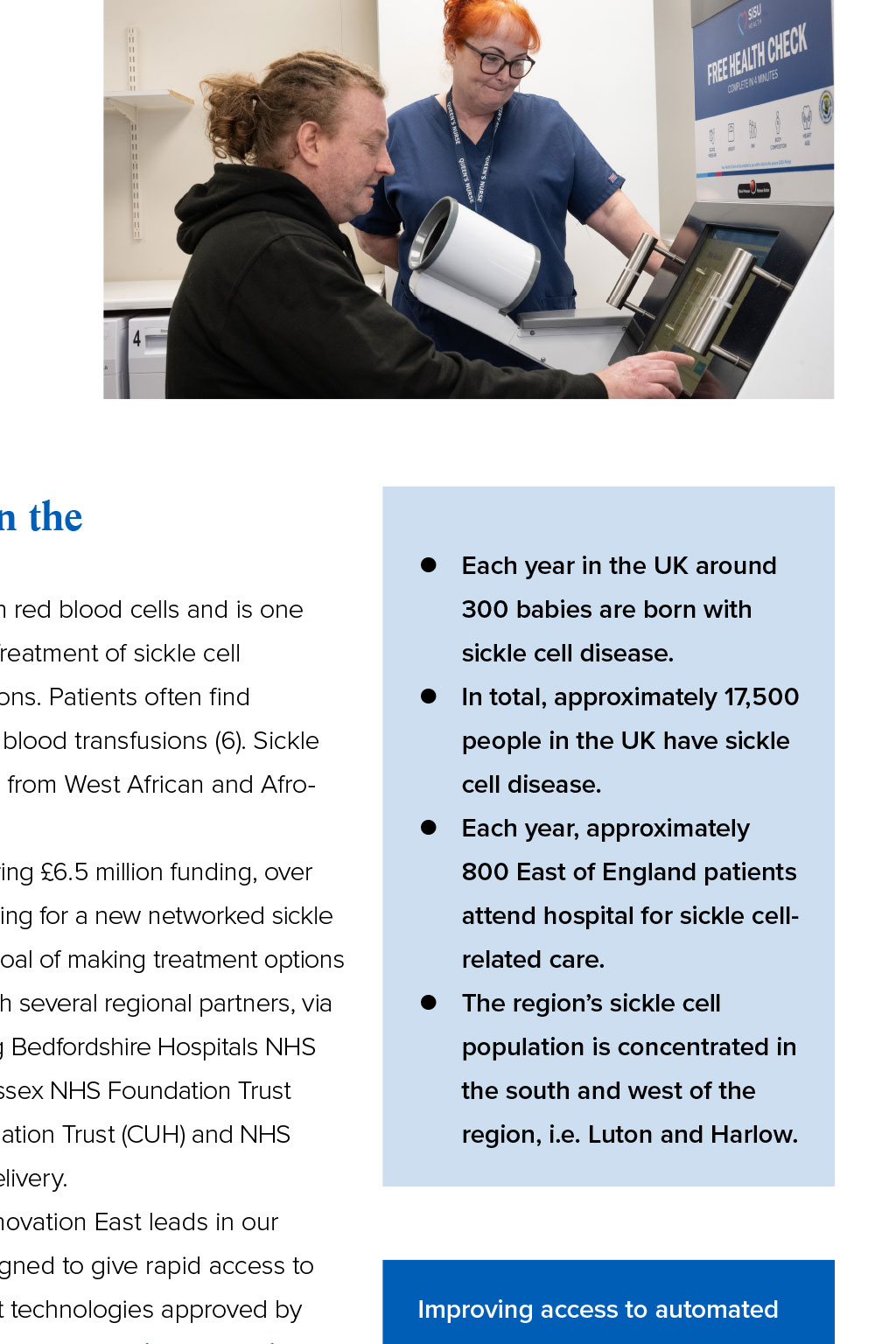
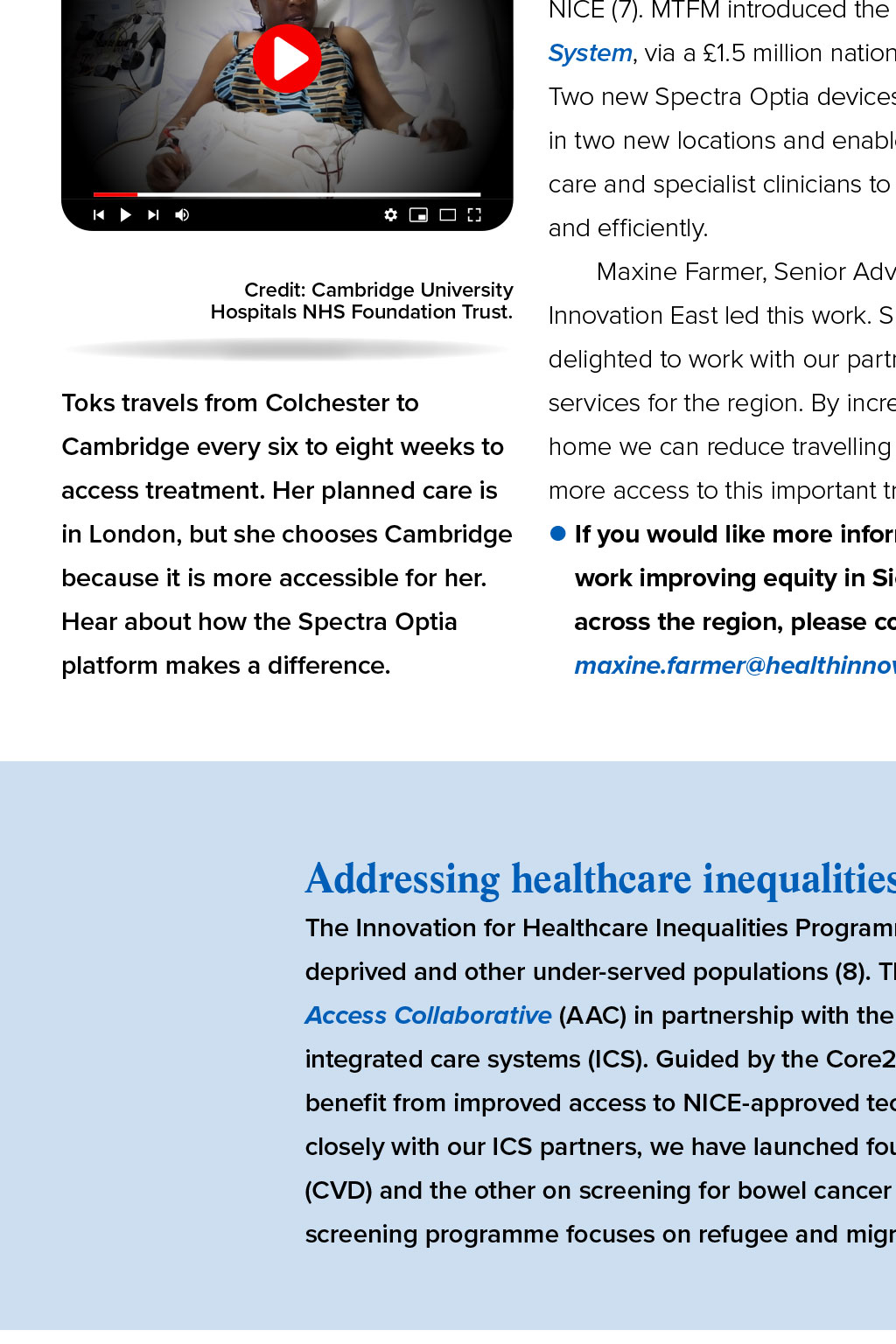


Innovation where it is most needed Helen Oliver, our Deputy CEO, shares examples of how we support innovations that address health inequalities in the East of England. Sir Michael Marmot, in his report Fairer Society, Healthy Lives (1), asserts that inequalities in health arise because of inequalities in society namely the conditions in which people are born, grow, live, work and age. In The Marmot Review 10 Years On (2), he continues that outcomes are even worse for minority ethnic population groups and people with disabilities. Addressing health inequalities is core to our work we aspire for the best innovations in health and care to reach the people, places and problems where they are most needed. We gather evidence, borne out in practice, to help understand how innovation makes a positive difference to peoples lives and to ensure that the innovations we support will not further entrench health inequity and healthcare inequality. Addressing health inequalities with data-driven insights Health and care practitioners and academics have decades worth of evidence about the causes of health inequalities. Yet there has been little progress in addressing them. In other words, we know why these inequalities exist, but there is much less evidence on what actually works to reduce them. The past 12 months have also seen us contribute to the establishment of the Health Equity Evidence Centre (HEEC). Stemming from a partnership with the NHS England East of England Primary Care Transformation team, and led by Dr John Ford, the HEEC is a hub providing evidence-informed solutions for equitable health and care (3). The researchers, practitioners and computer scientists involved are using innovative AI-based methodologies to build a robust evidence base of what works to address health and care inequalities. Their work focuses on primary care (where 90% of patient contact with the NHS takes place) and making the evidence they gather as accessible as possible to clinicians. Dr John Ford, Director of Read more about this work in our blog Health Equity Evidence Centre Dr Gary Howsam, chief clinical improvement officer at Cambridgeshire and Peterborough ICB and non-executive director at Health Innovation East, sees the impact of health inequalities every day. Of the HEEC, he says: Having an evidence-based, collective understanding of where to focus efforts for maximum impact is invaluable. Utilising this knowledge to enable primary care teams to concentrate their efforts on the areas which the evidence shows will lead to wins for their population will help maintain engagement and momentum and widen participation in this important work. Core20 5 PLUS people living in the other 20% most deprived areas of England excluded / disadvantaged groups as defined by the Index of Multiple Deprivation as recognised by the locality clinical priority areas CVD Maternity Severe mental illness Chronic respiratory conditions Early cancer diagnosis Core20PLUS5 is a national NHS England approach to inform action on healthcare inequalities. Partnering with patients to catalyse commercial success An important thread in our work is that we listen carefully and encourage others to engage purposefully with patients. Importantly, working this way shapes how innovations are developed and implemented, as our health and care systems should work for everyone. Enabling capacity with tech-enabled solutions Beacon House Ministries is a day centre for the homeless in Colchester. Among its valuable services the centre operates a drop-in clinic which sees up to 15 patients a day. Homeless people are particularly affected by health inequalities; evidence shows that health outcomes for the homeless are worse than those of the general population. A higher risk of mortality for the homeless is often coupled with long-term health conditions caused by mental health challenges and conditions such as cardiovascular disease (5). This year, recognising a shared goal of tackling inequalities with effective tech-enabled solutions, we connected Beacon Houses The SiSU health station is like an additional member of staff and most importantly encourages service users to learn more about and take greater ownership of their health status and outcomes advanced nurse practitioner, Michelle Wilkinson, to SiSU Health. Conversations led to SiSU placing one of its health stations at the centre, Michelle Wilkinson, advanced nurse practitioner, Beacon House Ministries supporting the clinic. The SiSU Health Station is an internet-enabled medical device that allows people to undertake a free, self-service health check in less than five minutes. It measures blood pressure, heart rate, body fat, height, BMI, weight, smoking status and even stress levels. The data the station collects can be emailed to Michelle, other healthcare professionals or to the person taking the test. Since its introduction, the health station has become an integral part of the clinic. It is available to anyone visiting the centre, anytime, and a trained volunteer is always on hand to offer support. The introduction of the station was a game changer for Michelle, freeing up her time to help service users with their wider needs. Read more about this work in our blog Transforming sickle cell services in the East of England z Each year in the UK around Sickle cell disease is a disorder of the haemoglobin in red blood cells and is one 300 babies are born with of the most common genetic conditions in England. Treatment of sickle cell sickle cell disease. mostly focuses on prevention and treating complications. Patients often find z In total, approximately 17,500 themselves in and out of hospital and require regular blood transfusions (6). Sickle people in the UK have sickle cell disease has a disproportionate impact on people from West African and Afro- cell disease. Caribbean communities. z Each year, approximately During 2023/24, we played an integral role in securing 6.5 million funding, over 800 East of England patients five years, from NHS England Specialised Commissioning for a new networked sickle attend hospital for sickle cell- cell service in the East of England. With the common goal of making treatment options related care. available where they are most needed, we worked with several regional partners, via z The regions sickle cell the NHS MedTech Funding Mandate (MTFM), including Bedfordshire Hospitals NHS population is concentrated in Foundation Trust (BHFT) and East Suffolk and North Essex NHS Foundation Trust the south and west of the (ESNEFT). Cambridge University Hospitals NHS Foundation Trust (CUH) and NHS region, i.e. Luton and Harlow. Blood and Transplant (NHSBT) have also supported delivery. The MTFM, which Health Innovation East leads in our region, is an NHS initiative designed to give rapid access to Credit: Cambridge University Hospitals NHS Foundation Trust. carefully selected, cost-efficient technologies approved by Improving access to automated NICE (7). MTFM introduced the Spectra Optia Apheresis red blood cell exchange therapy System, via a 1.5 million national investment in 25 devices. will increase the quality of life for Two new Spectra Optia devices are now available in the East patients, saving time and money in two new locations and enable patients to receive optimised and help provide a more optimal care and specialist clinicians to treat patients more effectively treatment closer to home. We and efficiently. are reducing health inequalities Maxine Farmer, Senior Advisor and MTFM Lead at Health Innovation East led this work. She says: I have been by creating a more equitable service across the region. delighted to work with our partners to develop sickle cell Toks travels from Colchester to services for the region. By increasing access to care closer to Cambridge every six to eight weeks to home we can reduce travelling time for patients and provide access treatment. Her planned care is more access to this important treatment. in London, but she chooses Cambridge If you would like more information our because it is more accessible for her. work improving equity in Sickle Cell services Hear about how the Spectra Optia across the region, please contact platform makes a difference. maxine.farmer@healthinnovationeast.co.uk Addressing healthcare inequalities locally The Innovation for Healthcare Inequalities Programme (InHIP) aims to address local healthcare inequalities experienced by deprived and other under-served populations (8). The programme was commissioned by NHS Englands Accelerated Access Collaborative (AAC) in partnership with the Health Innovation Network and offers funding and support to integrated care systems (ICS). Guided by the Core20PLUS5 planning framework, InHIP identifies groups of patients to benefit from improved access to NICE-approved technologies and develops an evidence base for their adoption. Working closely with our ICS partners, we have launched four initiatives in the region, with three focused on cardiovascular disease (CVD) and the other on screening for bowel cancer by supporting access to faecal immunochemical tests (FIT). The FIT screening programme focuses on refugee and migrant populations and people experiencing homelessness. Early cancer screening for bowel cancer in Norfolk and Waveney Nearly 43,000 people are diagnosed with bowel cancer every year in the UK and 54% of cases are preventable (9). Screening aims to find cancer, or changes in the bowel that could lead to cancer, at an earlier stage, when treatment is more likely to be successful. Public Health England, based on data from the Office for National Statistics (ONS), points to deaths from cancer being responsible for circa. 20% of the life expectancy gap between the least and most deprived communities and that underserved communities take up cancer screening programmes less than the mainstream population. This year, we worked alongside Norfolk and Waveney ICS to co-design the local bowel screening programme, providing comprehensive project and stakeholder management services. Focusing on improving screening uptake and working with community champions from eight voluntary sector organisations, the project team held 322 conversations with people from the target communities about ordering bowel screening tests. Insights from these conversations were analysed to help understand the barriers and enablers for accessing screening. 88 of the 322 people engaged expressed an intent to undergo bowel screening and participants reported an increased awareness of bowel cancer signs and symptoms. The programmes insights were well received by national and local services, informing future developments for bowel cancer screening. Share this article Return to About Us To discover more about how we help the best innovations to reach the people, places and problems where they are needed most, contact our deputy CEO, Helen Oliver helen.oliver@healthinnovationeast.co.uk Up next: How we are working to improve mental health for children and young people. References 1 Marmot, M. et al. (2010). Fair society, healthy lives: The Marmot Review. [Online]. www.instituteofhealthequity.org. Last Updated: February 2010. Available at: www. instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-exec-summary-pdf.pdf [Accessed 16 April 2024]. 2 Marmot, M. et al. (2020). Health Equity in England: The Marmot Review 10 year on. [Online]. www.insituteofhealthequity.org. Available at: www.instituteofhealthequity.org/ resources-reports/marmot-review-10-years-on/the-marmot-review-10-years-on-executive-summary.pdf [Accessed 16 April 2024]. 3 Ford, J. (2024). Welcome to the Health Equity Evidence Centre. [Online]. www.heec.co.uk. Last Updated: 31 January 2024. Available at: www.heec.co.uk/resource/welcome-tothe-health-equity-evidence-centre/ [Accessed 19 April 2024]. 4 NHS England. (2021). Core20PLUS5 (adults) an approach to reducing healthcare inequalities. [Online]. www.england.nhs.uk. Available at: www.england.nhs.uk/about/equality/ equality-hub/national-healthcare-inequalities-improvement- [Accessed 16 April 2024]. 5 Shelter. (2022). Two people died homeless every day last year. [Online]. www.england.shelter.org.uk. Last Updated: 23 November 2022. Available at: england.shelter.org.uk/ media/press_release/two_people_died_homeless_every_day_last_year_#:~: [Accessed 19 April 2024]. 6 Sickle Cell Society. (2024). About Sickle Cell. [Online]. www.sicklecellsociety.org. Available at: www.sicklecellsociety.org/about-sickle-cell/ [Accessed 16 April 2024]. 7 NHS England. (2024). MedTech Funding Mandate and MedTech Support. [Online]. www.england.nhs.uk. Available at: www.england.nhs.uk/aac/what-we-do/how-can-the-aachelp-me/the-medtech-funding-mandate/ [Accessed 16 April 2024]. 8 NHS England. (2022). Innovation for Healthcare Inequalities Programme. [Online]. www.england.nhs.uk/aac. Last Updated: October 2022. Available at: www.england.nhs.uk/ aac/what-we-do/innovation-for-healthcare-inequalities-programme/ [Accessed 16 April 2024]. 9 Cancer Research UK. (2024). Bowel cancer statistics. [Online]. www.cancerresearchuk.org. Available at: www.cancerresearchuk.org/health-professional/cancer-statistics/ statistics-by-cancer-type/bowel-cancer [Accessed 16 April 2024].