

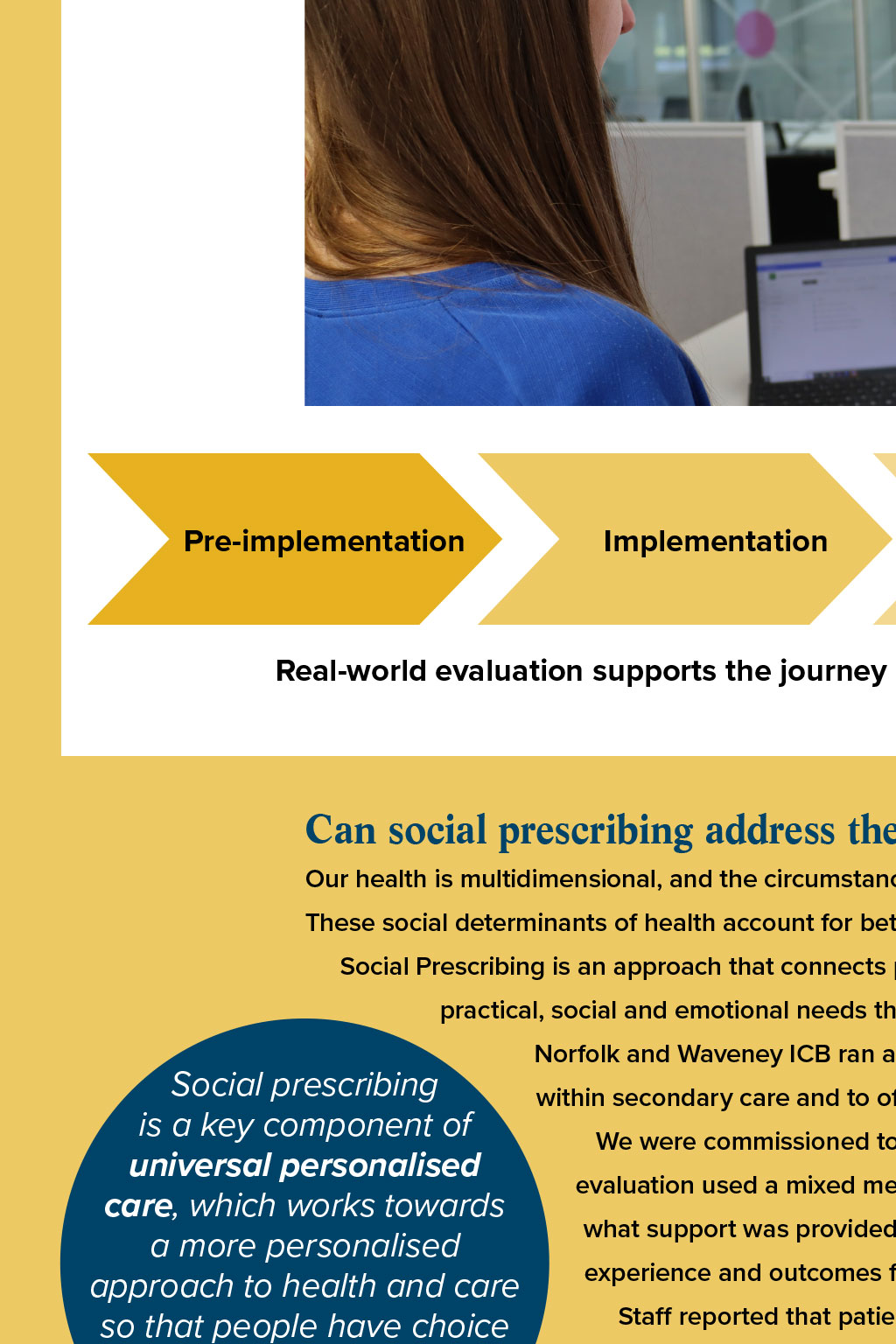



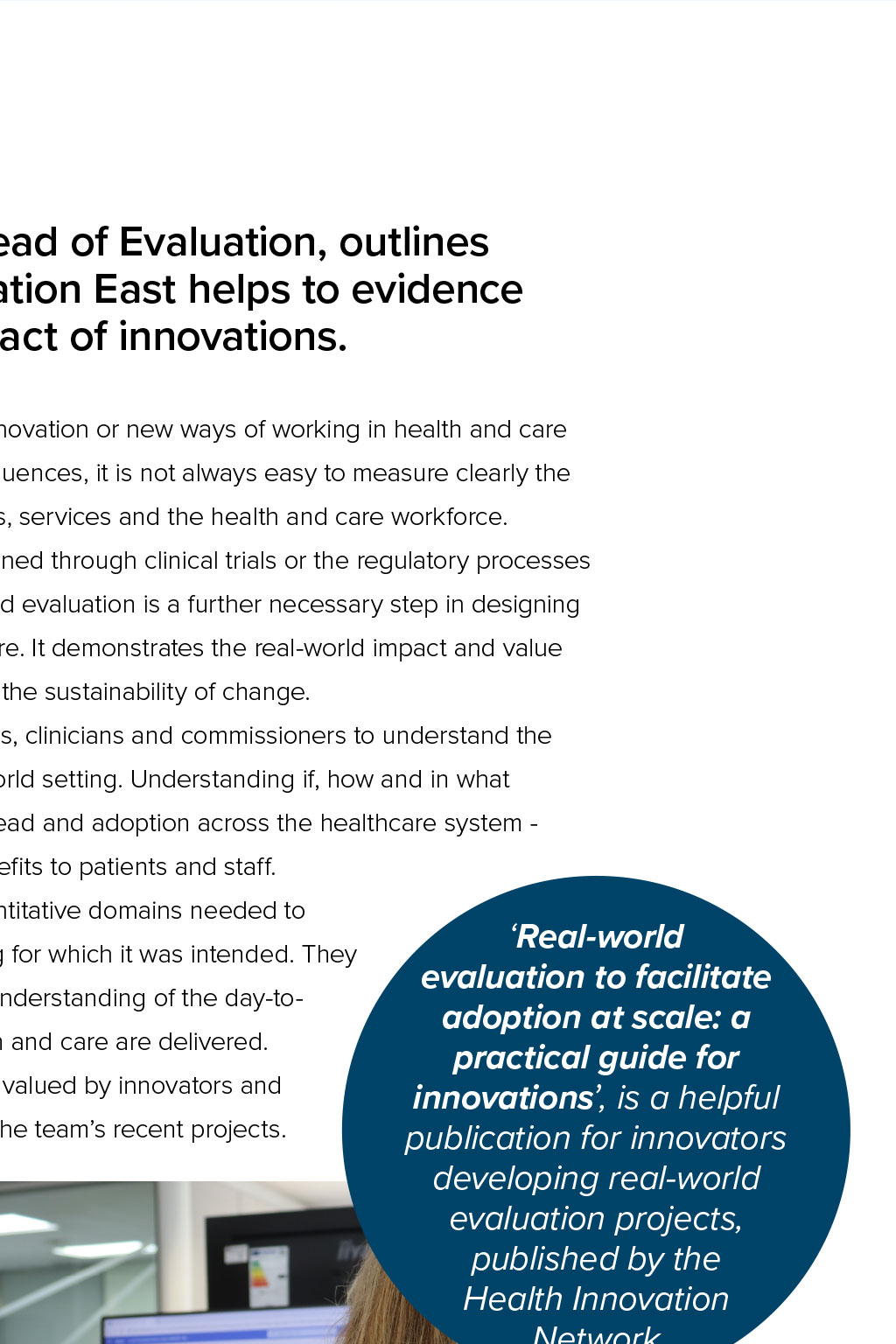

Developing evidence to understand impact Dr Judith Fynn, Head of Evaluation, outlines how Health Innovation East helps to evidence the real-world impact of innovations. Developing and implementing an innovation or new ways of working in health and care is often complex. With so many influences, it is not always easy to measure clearly the impact of an innovation on patients, services and the health and care workforce. The role of safety approvals gained through clinical trials or the regulatory processes is well known. However, real-world evaluation is a further necessary step in designing and implementing innovations in health and social care. It demonstrates the real-world impact and value of innovations or developments in practice to ensure the sustainability of change. Our real-world evaluation team can help innovators, clinicians and commissioners to understand the value of a new product or way of working in a real-world setting. Understanding if, how and in what contexts an innovation works is critical to help its spread and adoption across the healthcare system increasing best practice and bringing evidenced benefits to patients and staff. The team has expertise in the qualitative and quantitative domains needed to understand how an innovation performs in the setting for which it was intended. They combine academic expertise with a highly practical understanding of the day-today conditions, local and national, under which health and care are delivered. Their work is both rigorous and pragmatic and highly valued by innovators and commissioners alike. This article describes some of the teams recent projects. Pre-implementation Real-world evaluation to facilitate adoption at scale: a practical guide for innovations, is a helpful publication for innovators developing real-world evaluation projects, published by the Health Innovation Network Real-world evaluation Implementation Adoption and spread Real-world evaluation supports the journey of any innovation to adoption and spread Can social prescribing address the root causes of health issues? Our health is multidimensional, and the circumstances in which we are born, grow, live, work and age impact on our health. These social determinants of health account for between 30-55% of health outcomes (1). Social Prescribing is an approach that connects people to activities, groups and services in their community to meet the practical, social and emotional needs that affect their health and wellbeing. Social prescribing is a key component of universal personalised care, which works towards a more personalised approach to health and care so that people have choice and control over their mental and physical health. Norfolk and Waveney ICB ran a pilot, funded by NHS England, to integrate a social prescribing service within secondary care and to offer one-off personal health budgets. We were commissioned to conduct a real-world evaluation of the 12-month pilot project. The evaluation used a mixed methods approach to identify who was accessing the service, understand what support was provided to patients and explore the process of implementation through staff experience and outcomes for patients, the service and the wider system. Staff reported that patients needs were met for 98% of referrals made, supporting either admission avoidance or expedited discharge with an average of 5.3 bed days saved per patient. Re-admission rates over 90 days were also lower compared with other Norfolk & Waveney emergency admission rates. The findings highlighted the importance of improved integration of the service within the broader healthcare system, emphasising the need for staff support at all levels. To ensure the sustainability of the service the evaluation demonstrated the importance of securing continuous funding, facilitating strategic conversations and prioritising a standardised evaluation process, which should include recording the costs and savings associated with delivering the service. Read the report here An evaluation of a separate social prescribing project, commissioned by South Norfolk and Broadland Health and Wellbeing Partnership, also emphasised the potential of social prescribing to support the sustainability of services. Read the report here Measuring the impact of innovations that tackle high blood pressure 30% of adults in the UK are estimated to have hypertension (high blood pressure) - with approximately 6-8 million people living with undiagnosed or uncontrolled high blood pressure (2). Uncontrolled hypertension can lead to serious damage to the heart, put patients at risk of suffering a stroke and can cause kidney damage, eye disease and some types of dementia (3) (4). By using new technologies or care pathways, we can facilitate diagnosis and improve management of hypertension to help prevent potentially life-changing complications. Florence, created by Generated Health, is a personabased messaging system designed to support and encourage patients to self-manage their long-term condition. Staploe Medical Centre implemented Florence to provide patients with a way to take their blood pressure reading at home and get instant feedback. We were commissioned by Ely North and South Primary Care Network (PCN) to evaluate the implementation of the tool at Staploe Medical Centre to help inform spread and adoption of Florence across the PCN. The team used a mixed methods approach to assess the Health Innovation East led a thorough and in- depth evaluation, which demonstrated the benefits and implementation experiences embedding the Florence platform within Staploe Medical Centre. The findings are helping to scale implementation across Ely North and South PCN. Generated Health recommend Health Innovation East to other innovators for their outstanding expertise in delivering this evaluation, to the benefit of both the local system and the innovator. outcomes of the pilot and gain insights into how the process has worked for patients and professionals. Insights gathered John Griffiths, commercial director at Generated Health helped to inform our key recommendations to support wider implementation across Ely and North and South PCN including: the need to develop and share educational materials for both patients and staff, provide clear engagement strategies to onboard patients and support staff to feel comfortable promoting the platform. ExpertCare AI (ExpertCare) is a medicines optimisation tool that promotes adherence to the National Institute for Health Care and Excellence (NICE) guidelines on the management of hypertension and its most prevalent comorbidities, such as diabetes and cardiovascular disease. It is being piloted across several practices and PCNs in England. We have evaluated its implementation to understand where the tool could improve medication compliance when treating hypertension. To achieve this we analysed data captured by the ExpertCare system to explore different experiences across subgroups of patients. While we found no significant differences with ExpertCare in compliance, or changes in compliance following review, due to a high level of compliance in the sample prior to using ExpertCare, the data showed that ExpertCare is a quick and easy system for clinicians to use to confirm compliance and complete hypertensive reviews and has the potential to improve blood pressure management. Read our evaluation of Florence here Building evaluation into app development Digital technologies are helping to bridge the demand-supply gap in healthcare, playing a key role in tackling growing waiting lists, reducing health inequalities and improving access to care, treatment and support. There is a growing demand for mental health services in England, with a record 5 million referrals received during 2023 (up 33% from 2019) (5). In response, digital technologies are helping to redefine the approach to supporting and caring for mental health to address this need. Seren is a therapeutic app-based tool developed by Lumino to provide self-guided cognitive behaviour therapy (CBT) for anyone dealing with menopause symptoms. It is estimated that there are around 13 million people who are currently peri-menopausal or menopausal in the UK, including 2.5 million people currently experiencing significant symptoms associated with menopausal transition (6) (7). 50% of people say it has had a negative impact on their mental health (7). Seren has been designed to make CBT much more affordable and accessible for those who could benefit. Health Innovation East conducted a qualitative evaluation of Seren during the launch of their beta testing trial. 30 participants were given access to the Seren app for three weeks and interviewed following the end of their trial period. The evaluation focused on four core areas: the impact of menopause symptoms, diagnosis and treatments of the participants, participants usage and experience of the app. The evaluation found that participants enjoyed using the app, it was informative, reassuring and validating. Although, the evaluation highlighted that using a more diverse sample of people living with menopause would be beneficial, it also highlighted that users would like to be able to track their progress. The insights gathered from the evaluation will be instrumental in the next stage of the development of Seren to ensure we are best supporting people going through menopause. It has been a brilliant experience working with Health Innovation East throughout the evaluation process, and their leadership and insights have been second to none. Becky Cotton, Lumino co-founder How we can support you Our real-world evaluation team can support you in planning and completing evaluations, helping to broaden the evidence base for your innovation and by providing valuable insights to inform commissioning, service development, and scalability. Share this article Return to About Us We can play a leading role in your real-world evaluation or provide tailored support and guidance. Find out more about how we can support your evaluation needs by emailing evaluations@healthinnovationeast.co.uk or visiting our website. Up next: Read how we are working with our partners in the region to reduce health equalities across the population. References 1 World Health Organisation. (2024). Social determinants of health. [Online]. World Health Organisation. Available at: www.who.int/health-topics/social-determinants-of-health [Accessed 4 April 2024]. 2 British Heart Foundation. (January 2024). CVD statistics UK. [Online]. British Heart Foundation. Available at: www.bhf.org.uk/-/media/files/for-professionals/research/heartstatistics/bhf-cvd-statistics-uk-factsheet.pdf [Accessed 4 April 2024]. 3 NHS. (2023). High blood pressure. [Online]. NHS. Last Updated: 11 July 2023. Available at: www.nhs.uk/conditions/high-blood-pressure-hypertension [Accessed 4 April 2024]. 4 WedMD. (2022). High blood pressure and eye disease. [Online]. WedMD. Last Updated: 2 November 2022. Available at: www.webmd.com/hypertension-high-blood-pressure/ eye-disease-high-blood-pressure [Accessed 4 April 2024]. 5 BMA. (2024). Mental health pressures in England. [Online]. BMA. Last Updated: 3 April 2024. Available at: www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/ pressures/mental-health-pressures-data-analysis [Accessed 4 April 2024]. 6 NHS England. (2022). Menopause in the workplace. [Online]. Engage England. Available at: www.engage.england.nhs.uk/safety-and-innovation/menopause-in-the-workplace [Accessed 4 April 2024]. 7 Lumino. (2024). Seren Health. [Online]. Seren Health. Available at: www.seren.health [Accessed 4 April 2024].