

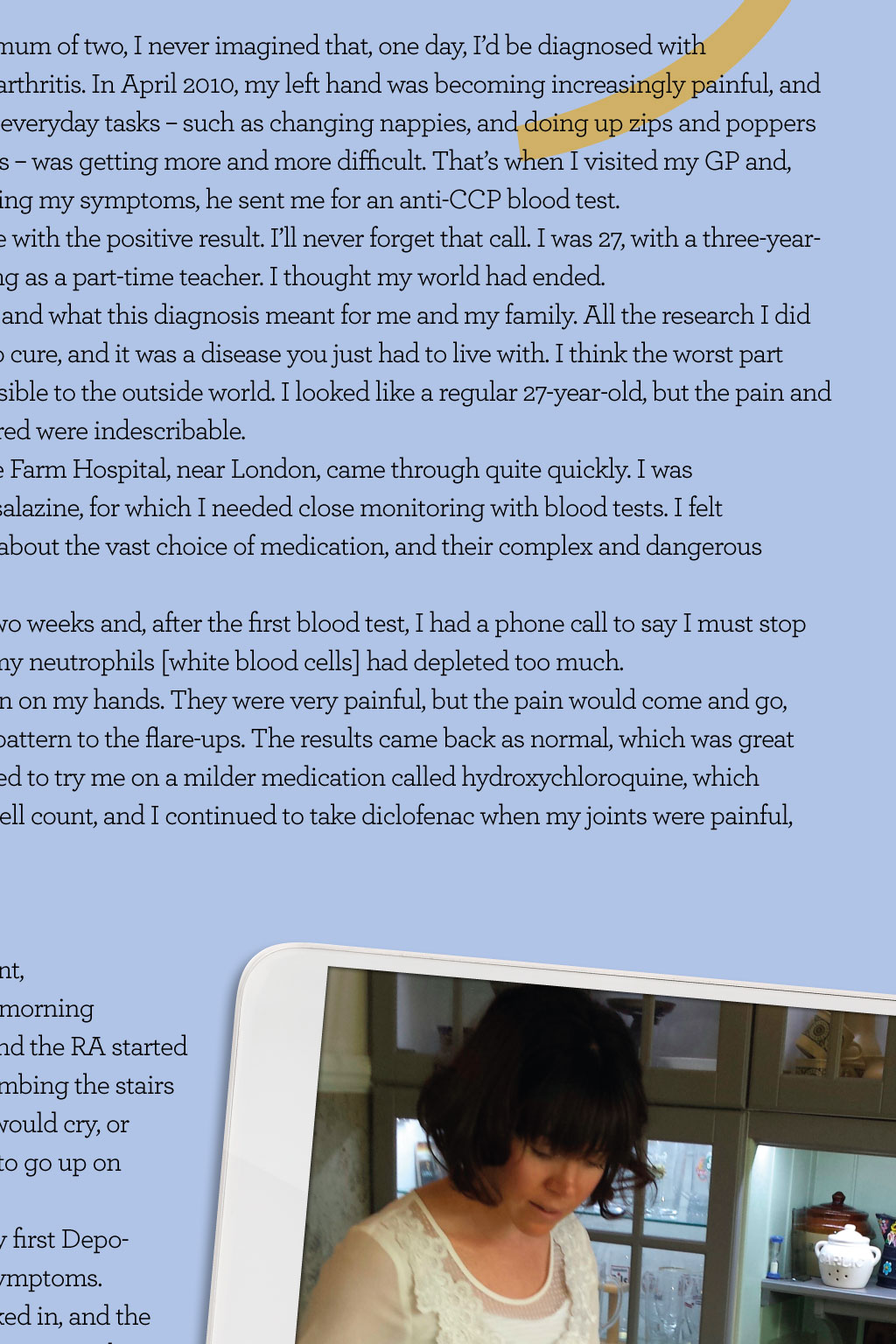

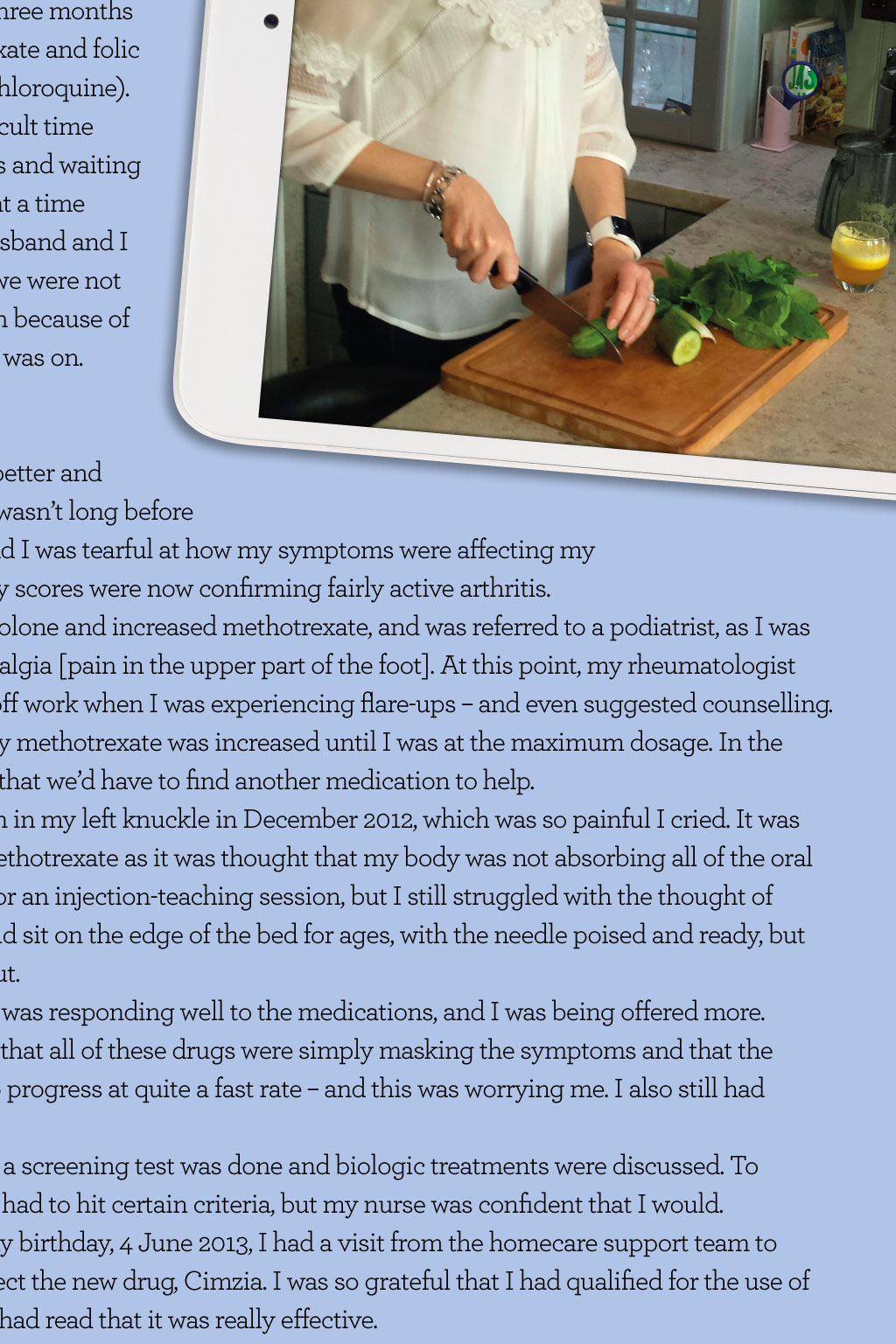
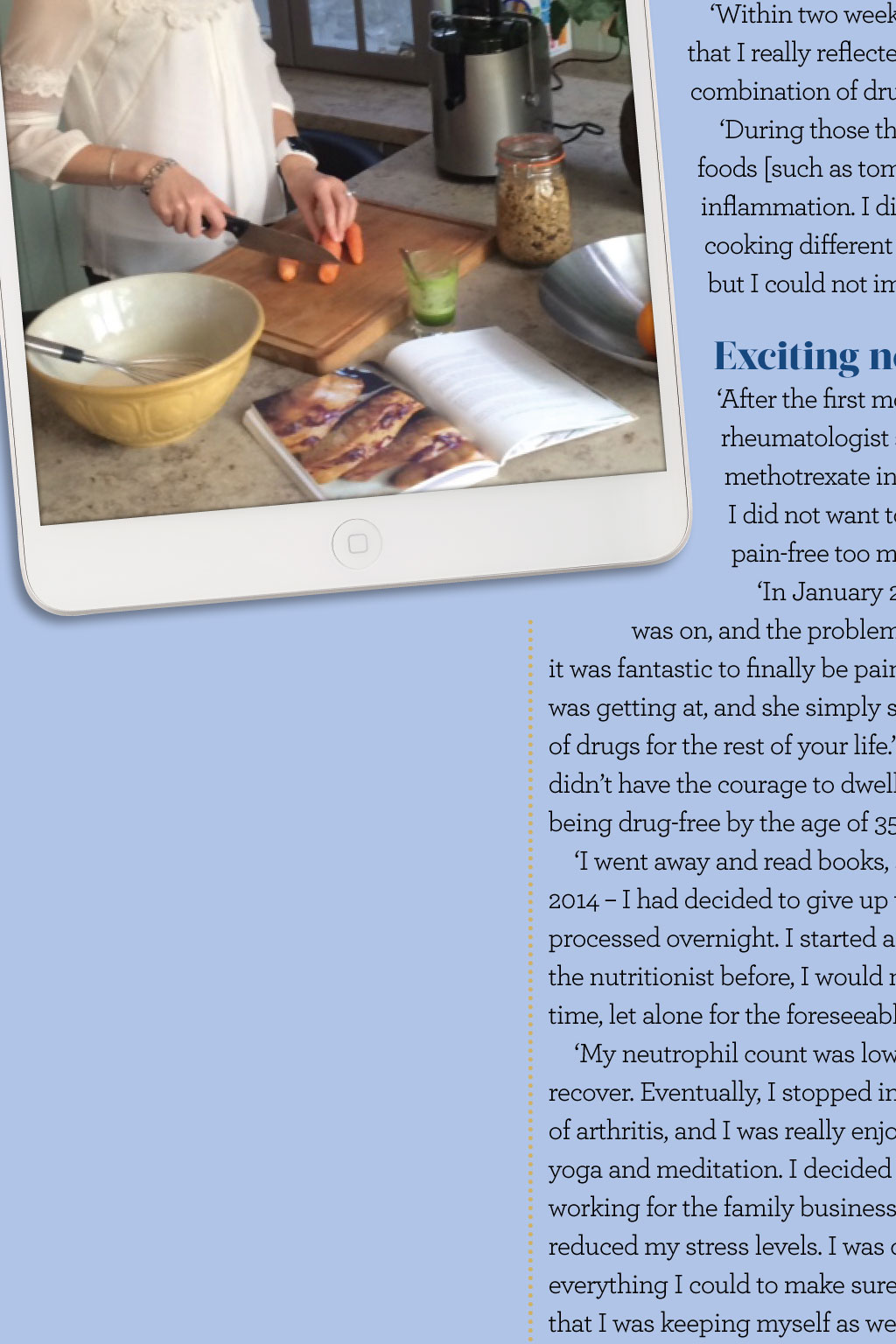
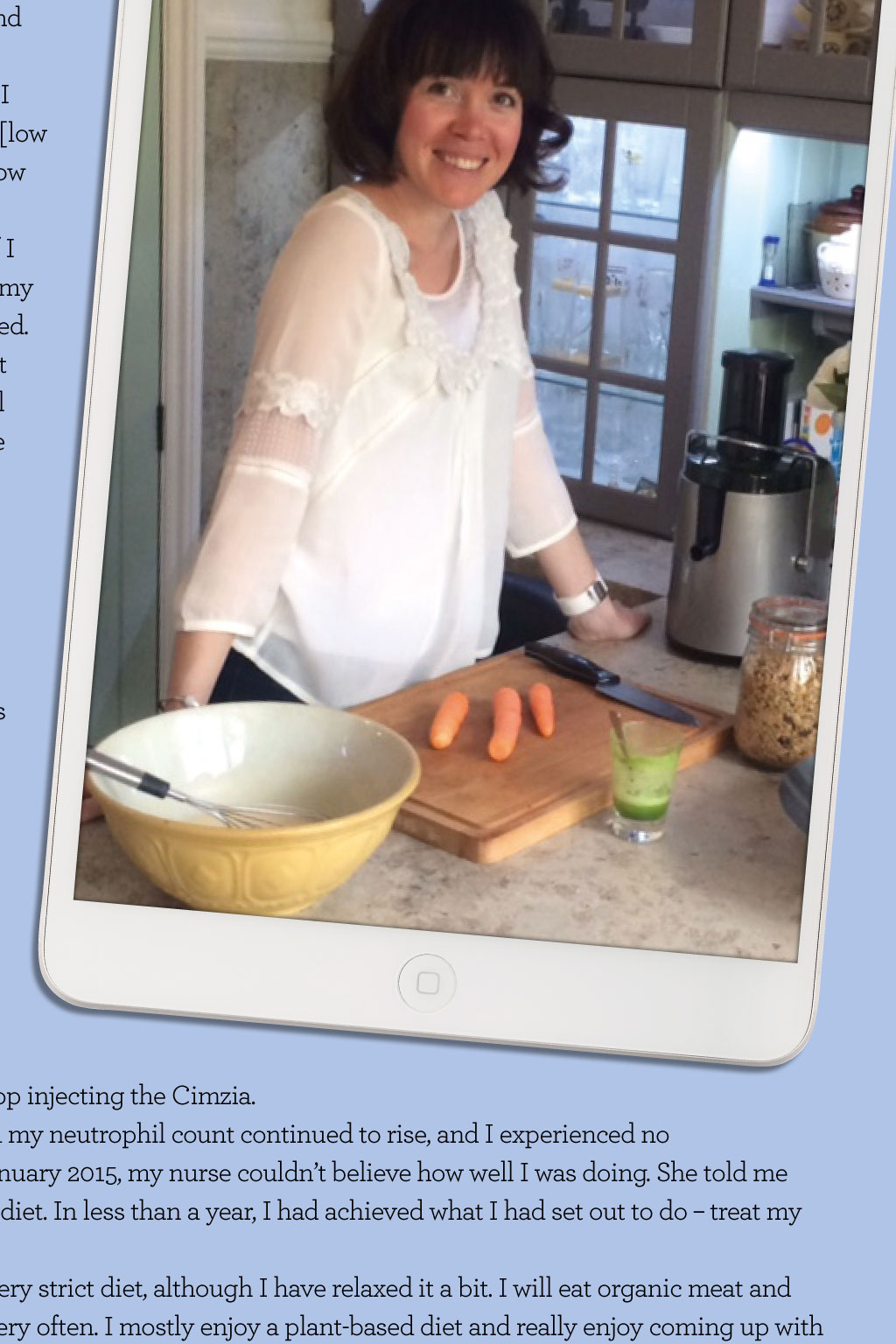


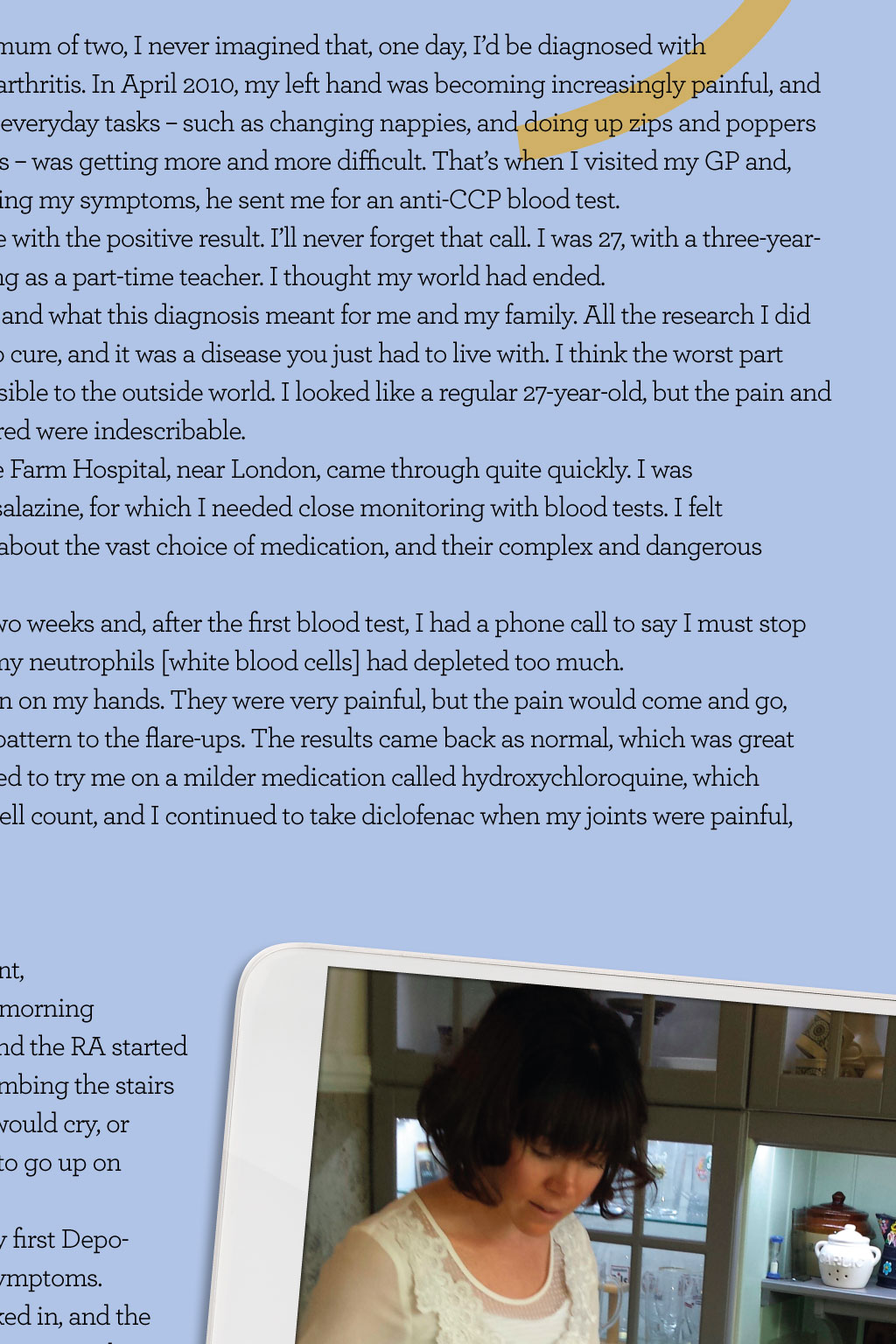

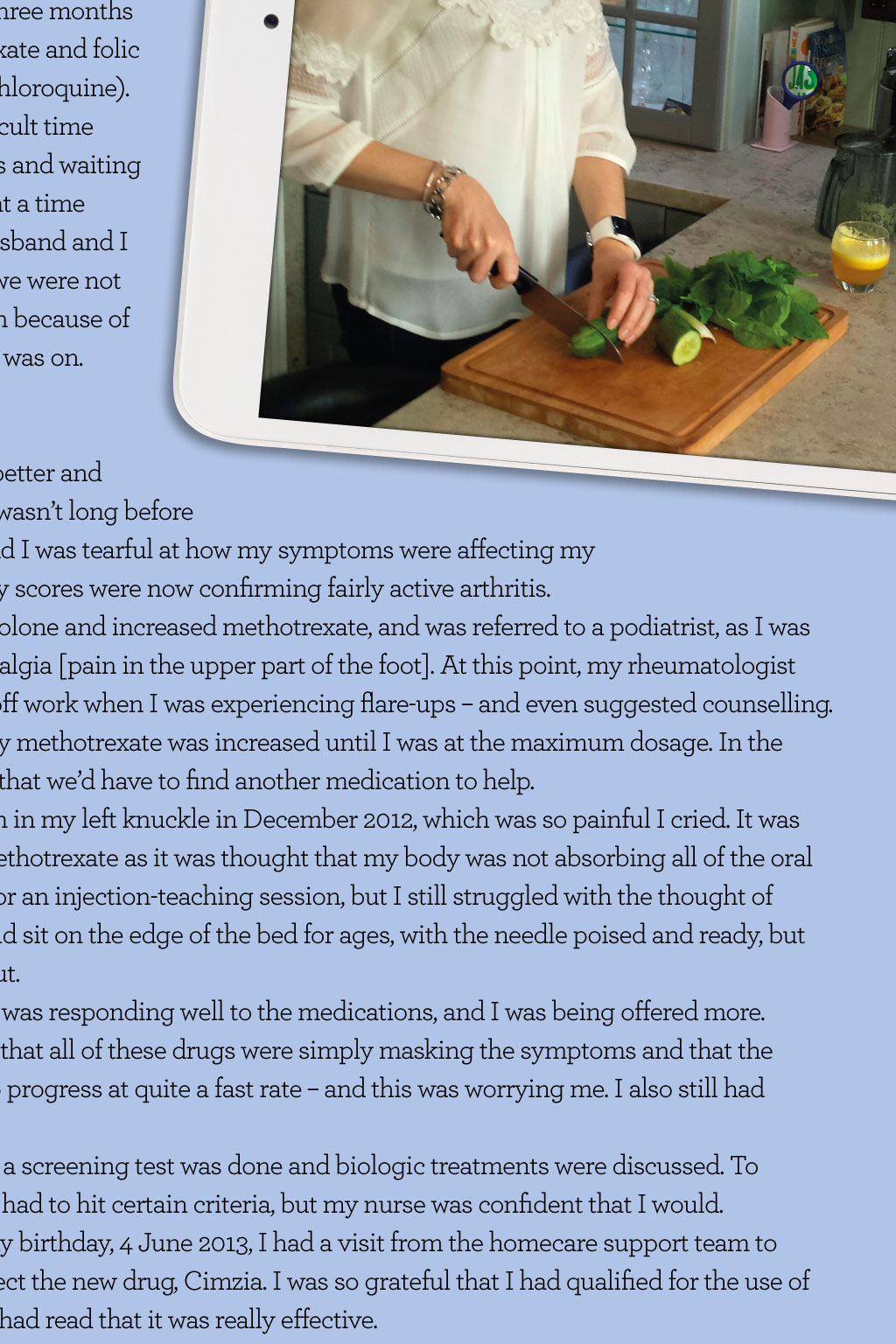
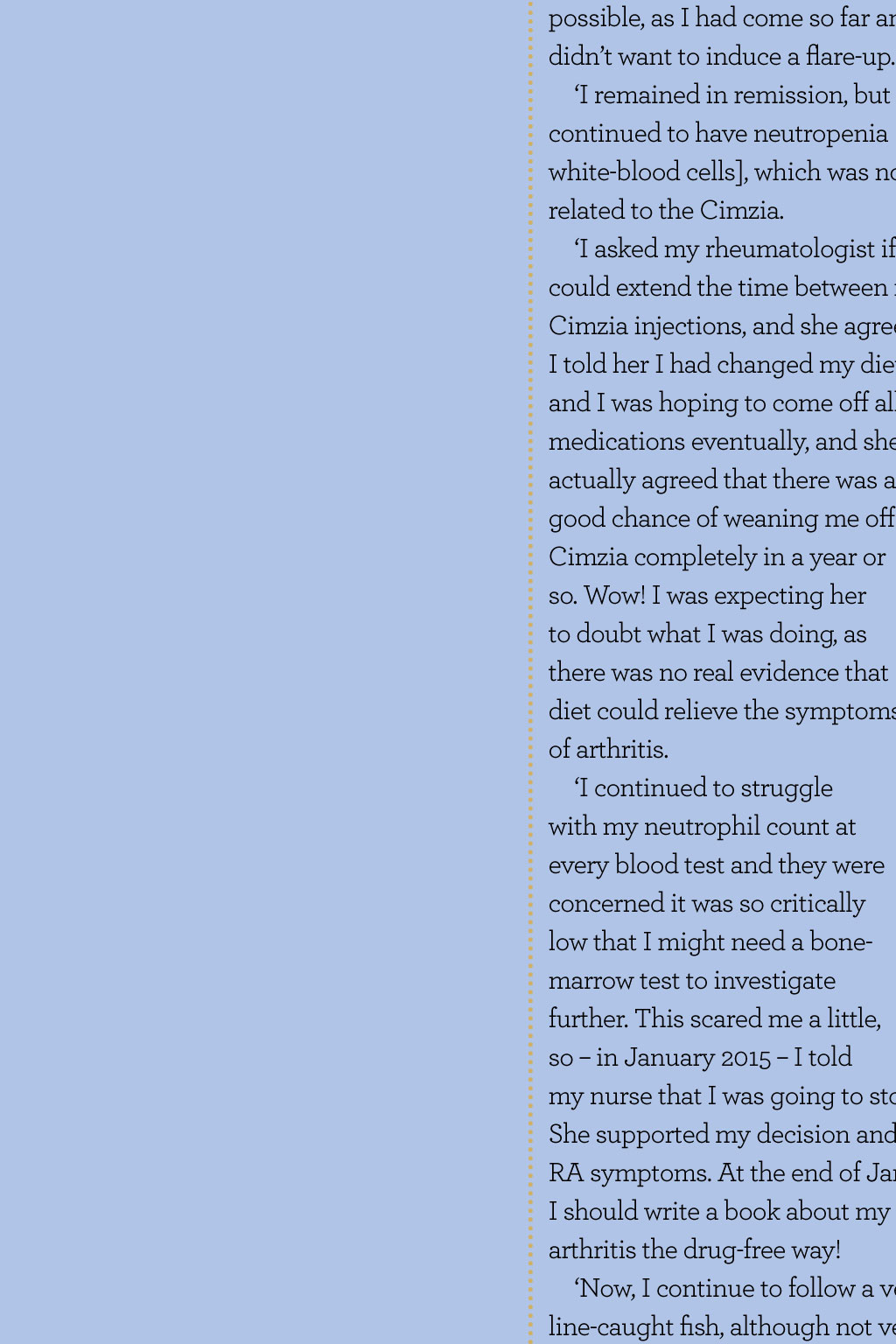
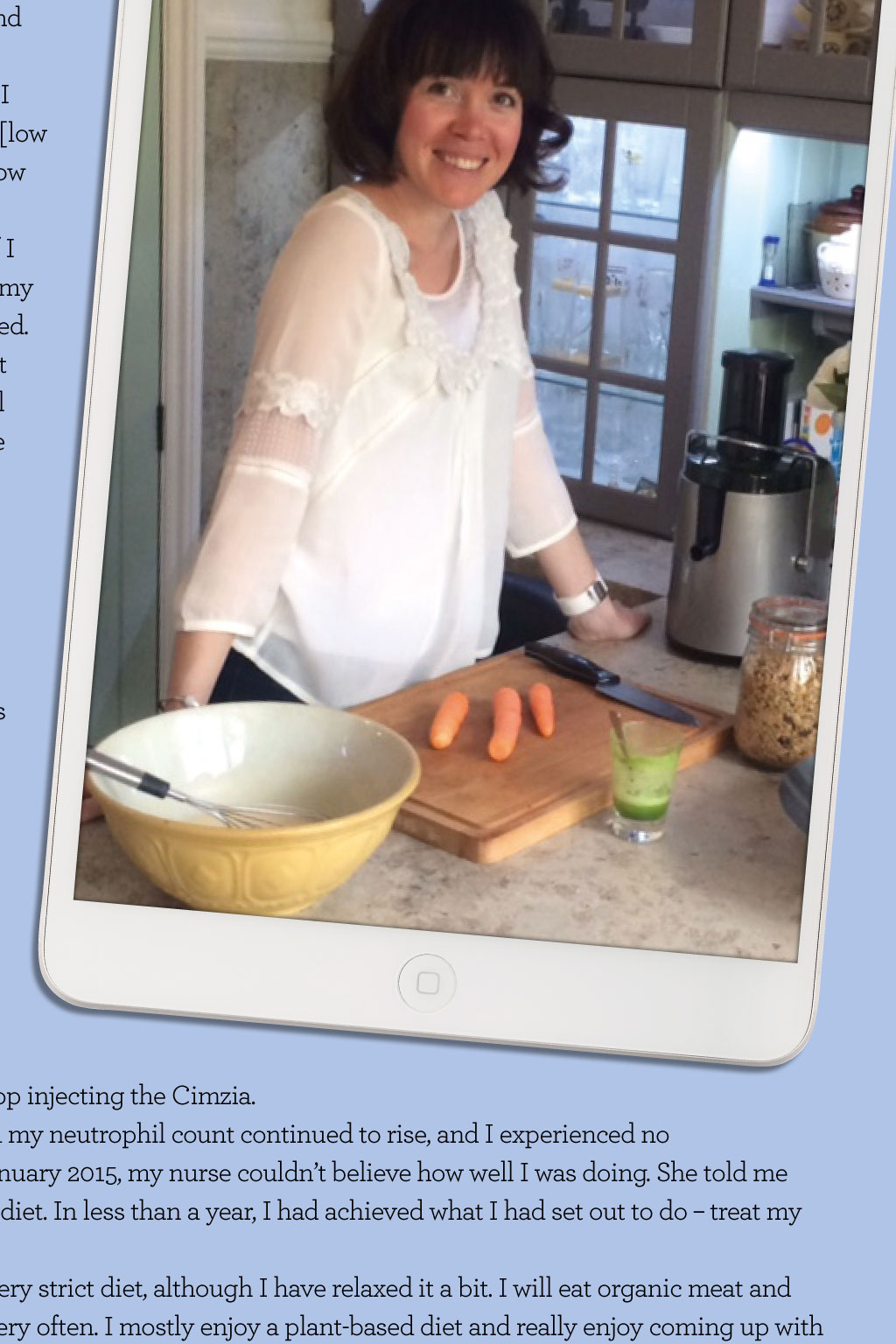
I thought my world had ended somerset King, 32, was a happy mum of two until a shock diagnosis revealed rheumatoid arthritis. However, she turned her life around thanks to hard work, dedication, and a better diet and lifestyle sAY Hello! Take a look at Somersets Facebook page, Purely Somerset, or email. Shed love to hear from you. B eing a busy mum of two, i never imagined that, one day, id be diagnosed with rheumatoid arthritis. in april 2010, my left hand was becoming increasingly painful, and carrying out everyday tasks such as changing nappies, and doing up zips and poppers on sleep suits was getting more and more difficult. Thats when i visited my GP and, after describing my symptoms, he sent me for an anti-CCP blood test. a few days later, he phoned me with the positive result. ill never forget that call. i was 27, with a three-yearold and an 18-month-old, working as a part-time teacher. i thought my world had ended. i was worried about the future and what this diagnosis meant for me and my family. all the research i did was clear in stating there was no cure, and it was a disease you just had to live with. i think the worst part about the disease is that its invisible to the outside world. i looked like a regular 27-year-old, but the pain and tiredness i eventually encountered were indescribable. my first appointment at Chase Farm Hospital, near London, came through quite quickly. i was immediately prescribed sulphasalazine, for which i needed close monitoring with blood tests. i felt overwhelmed with information about the vast choice of medication, and their complex and dangerous sideeffects. i took the sulphasalazine for two weeks and, after the first blood test, i had a phone call to say i must stop taking it immediately because my neutrophils [white blood cells] had depleted too much. i was then sent for an mRi scan on my hands. They were very painful, but the pain would come and go, andthere seemed to be no real pattern to the flare-ups. The results came back as normal, which was great news. my rheumatologist decided to try me on a milder medication called hydroxychloroquine, which wouldnot cause the low white-cell count, and i continued to take diclofenac when my joints were painful, which really helped. Testing times at each subsequent appointment, i had tender and swollen joints, morning stiffness and severe tiredness, and the Ra started affecting my knees and feet. Climbing the stairs in the evening was so painful i would cry, or it would be so impossible i had to go up on mybottom. in august 2011, i was given my first Depomedrone injection to ease my symptoms. This seemed to help once it kicked in, and the effects lasted for a little while. Three months later, i was prescribed methotrexate and folic acid (i was still taking hydroxychloroquine). starting medications was a difficult time for me, with constant blood tests and waiting in the blood-test unit for hours at a time with two young children. my husband and i had to decide at this point that we were not going to have any more children because of the strength of the medication i was on. Feeling tearful I had nally found a combination of drugs that had the RA under control By January 2012, i was feeling better and had no side effects. However, it wasnt long before i was suffering with stiffness, and i was tearful at how my symptoms were affecting my everyday life. my disease activity scores were now confirming fairly active arthritis. i was prescribed oral prednisolone and increased methotrexate, and was referred to a podiatrist, as i was experiencing constant metatarsalgia [pain in the upper part of the foot]. at this point, my rheumatologist recommended that i take time off work when i was experiencing flare-ups and even suggested counselling. over the next few months, my methotrexate was increased until i was at the maximum dosage. in the back of my mind, i was worried that wed have to find another medication to help. i was given a steroid injection in my left knuckle in December 2012, which was so painful i cried. it was suggested that i try injecting methotrexate as it was thought that my body was not absorbing all of the oral dosage. i was booked for an injection-teaching session, but i still struggled with the thought of injecting myself. i would sit on the edge of the bed for ages, with the needle poised and ready, but hesitating to carry it out. By February 2013, i was responding well to the medications, and i was being offered more. However, i was aware that all of these drugs were simply masking the symptoms and that the Ra was continuing to progress at quite a fast rate and this was worrying me. i also still had lowneutrophils. Two months later, a screening test was done and biologic treatments were discussed. To qualify for funding, i had to hit certain criteria, but my nurse was confident that i would. The day before my birthday, 4 June 2013, i had a visit from the homecare support team to teach me how to inject the new drug, Cimzia. i was so grateful that i had qualified for the use of this drug because i had read that it was really effective. Within two weeks, i felt so much better. it wasnt until i was totally pain-free for a few months that i reallyreflected on the pain i had beenin for just over three years. i had finally founda combination of drugs that had the Ra under control, and i felt like myself again. During those three years, i saw a nutritionist who recommended that i avoid all nightshade foods [such as tomatoes, peppers and aubergines] as there were reports of them causing inflammation. i did this for two months, but i felt no different, and found it very difficult cooking different meals for myself and my family. The next step was to try an elimination diet, but i could not imagine a life giving up wheat and dairy, so i didnt pursue it. Exciting news after the first month of Cimzia, my Ra was in remission. i couldnt believe it! my rheumatologist stopped the hydroxychloroquine, and then she suggested reducing the methotrexate in six months time if i remained in remission. The idea of this scared me, as i did not want to reduce my medications and experience a flare-up i was enjoying being pain-free too much. in January 2014, i went to see my Pilates teacher and we discussed the medication i was on, and the problems i was having with my low neutrophils. she asked me how i felt and i said it was fantastic to finally be pain free. Her answer was yes, but what now? i didnt understand what she was getting at, and she simply said: Well, what are you going to do now? you cant be on that combination of drugs for the rest of your life. Wow, that was a shock realisation! i had been having thoughts about it, but didnt have the courage to dwell on it too much. We discussed trying to reduce my drugs with the hope of being drug-free by the age of 35. i went away and read books, searched the internet and came across various blogs, and by February 2014 i had decided to give up wheat, gluten, cows milk products, meat, fish, refined sugar and anything processed overnight. i started a very strict plant-based, alkaline diet. its so strange to think that, when i saw the nutritionist before, i would not even attempt the idea of giving up so much for even a short amount of time, let alone for the foreseeable future. its amazing how determined i was. my neutrophil count was low again and i was advised to stop injecting for a while, to let my body recover. eventually, i stopped injecting methotrexate in July 2014. i continued to feel great, with no signs of arthritis, and i was really enjoying my new diet and lifestyle. i was continuing with Pilates and took up yoga and meditation. i decided to leave teaching and started working for the family business, which reduced reduced my stress levels. i was doing everything i could to make sure that that i was keeping myself as well as possible, as i had come so far and didnt want to induce a flare-up. i remained in remission, but i continued continued to have neutropenia [low white-blood cells], which was now related to the Cimzia. i asked my rheumatologist if i could could extend the time between my Cimzia Cimzia injections, and she agreed. i told her i had changed my diet and i was hoping to come off all medications eventually, and she actually agreed that there was a good chance of weaning me off Cimzia completely in a year or so. Wow! i was expecting her to doubt what i was doing, as therewas no real evidence that diet could relieve the symptoms of arthritis. i continued to struggle with my neutrophil count at every blood test and they were concerned it was so critically low that i might need a bonemarrow test to investigate further. This scared me a little, so in January 2015 i told my nurse that i was going to stop injecting the Cimzia. she supported my decision and my neutrophil count continued to rise, and i experienced no Ra symptoms. at the end of January 2015, my nurse couldnt believe how well i was doing. she told me i should write a book about my diet. in less than a year, i had achieved what i had set out to do treat my arthritis the drug-free way! Now, i continue to follow a very strict diet, although i have relaxed it a bit. i will eat organic meat and line-caught fish, although not very often. i mostly enjoy a plant-based diet and really enjoy coming up with new recipes. i dont crave anything, and my children and family are very supportive. my vision now is to try to share my story so that i can help others deal with the crippling effects of Ra i hope it inspires others. everyone is different, and my dietwont work for all, but id like to think my story would spark a change insomeone to try to take control of thedisease instead of letting it controlthem.